Omega-3s: a review of the recent evidence – part one
Few nutrients have been studied as extensively as omega-3 fatty acids, with evidence-based research supporting the link between omega-3 insufficiency and the risk for chronic disease. As essential nutrients, the long-chain omega-3s eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are especially relevant as they are not only required to support normal growth and development, but they also play a role in supporting immune function and the maintenance of cardiovascular health, as well as direct and essential roles in regulating inflammatory processes. [1, 2] Chronic low-grade inflammation is now recognised to be a contributor to cardiovascular disease (CVD) and to play a role in numerous additional diseases like type II diabetes, liver disease and cognitive decline. In 2018 we saw the publication of studies supporting omega-3 in mood, cognitive decline, for healthy pregnancy outcomes and for liver health, as well as many other areas. What is clear is that the effects of EPA and DHA on health outcomes are likely to be influenced by baseline levels and are dose-dependent.
The most studied fatty acid / disease relationship is between EPA & DHA and CVD and while the effects of omega-3 [extensively established by in vitro and animal models] are known to be both numerous and diverse in supporting health and reducing disease risk, these benefits are not always reflected by human dietary intervention studies, with the area of CVD particularly vulnerable to controversy. In 2018, several reviews and meta-analyses of omega-3 intervention studies reported negative or null findings which, for both practitioners and consumers, did nothing more than to feed the confusion surrounding the potential benefits that can be gained by including fish oils in the diet. [3, 4] As such, the ongoing controversy surrounding the use of omega-3 to support health and longevity continues.
As with many areas of nutrition research, all is not as it seems, and by conducting a deep dive into the research it is surprisingly easy to unravel what appear to be the continued and repeated flaws in the current methodology that, if acknowledged in future study design, would have the potential to show very different outcomes. For example, many cardiovascular studies are limited by design issues, including low dosage, poorly absorbed omega-3, no assessment of omega-3 status, and absence of a clear biological target or pathophysiologic hypothesis for the intervention (participants are often not considered to be at risk for the very reason the supplements are taken). These limitations are often exposed and heavily criticised [5, 6], and despite the negative messages that may arise from poorly designed studies, new research continues to support past studies showing that the Omega-3 Index is inversely related to risk for total mortality and fatal CVD events. [8] What seems clear is that those studies that address these issues, and especially those studies that report omega-3 status as a biomarker of disease risk and change in risk (so risk reduces as the omega-3 levels increases) show the most favourable outcomes that continue to support the benefits of omega-3 supplementation. If, however, the tendency to continually repeat the same mistakes in study design carries on, this will only serve to mask what are clear and overwhelming benefits that can be derived from increasing our intake of omega-3.
Nutrients are not drugs!
While observational studies show the protective benefits of high omega-3 status, we still need to ‘prove’ that raising omega-3 levels will confer protection against ill health. Randomised, controlled trials (RCTs) are still considered to be the most scientifically rigorous method of hypothesis testing available, and as such are the gold standard for evaluating the effectiveness of an intervention. The purpose of the RCT is to ensure that the only difference between groups is the intervention being compared. In the case of drug trials, exposure to a drug versus placebo (no drug) provides two clearly distinct groups that allow the efficacy of the drug being studied to be determined. In contrast, in nutrition trials, the efficacy of the nutrient of interest (the intervention) is significantly harder to assess because it is highly likely that both groups (placebo and active) will have had exposure to the nutrient prior to the trial (creating a baseline level for both groups), or that both groups will continue to have exposure to the nutrient (via uncontrollable ‘normal’ dietary intake) throughout the study. Thus, within dietary intervention studies, a true placebo group with absolutely no intake of the nutrient being studied is highly unlikely. Therefore, when considering omega-3 dietary interventions, there is no clear distinction between the two groups (placebo and omega-3) unless blood analysis pre- and post-supplementation is carried out. The value of testing can therefore not be overlooked, because it is the only way to identify the ‘at risk’ population best suited to the intervention (by ensuring baseline omega-3 status of the study participants is not too high), and to ensure that the dose used in the study is high enough to increase the ‘at risk’ individuals’ omega-3 status so that it will be high enough to be able to statistically assess the efficacy of omega-3 as an intervention. What is clear is that including subjects who achieve less than therapeutic blood levels will dilute the beneficial effect of omega-3 supplementation on clinical endpoints. The use of highly concentrated fish oil as re-esterified triglyceride (rTG) at a dose of ~20-25mg/kg is the most effective way of ensuring therapeutic blood levels of omega-3 are achieved. [8, 9]
Low-dose trials are not conducive to benefits
The most damaging review of Omega-3 published in 2018 compared 79 trials involving 112,059 people, and reported “little or no difference to risk of cardiovascular events, coronary heart deaths, coronary heart disease events, stroke or heart attack.” [1]. Yet only 40 of these studies were direct CVD intervention studies, with at least 23 studies using doses that could be considered too low for effect. For example, secondary prevention RCTs such as the Alpha Omega, OMEGA, SU.FOL.OM3, and ORIGIN studies [10-13] all used doses lower than 1g. In addition, a number of primary prevention studies, such as the Risk and Prevention, the ASCEND and the VITAL studies [14-16], also used omega-3 doses of 1g or less. In total, 17 of the 23 studies used an omega-3 dose of 1g or less with the majority of these using the less well absorbed ethyl-ester form that continues to be commonly used in research trials despite the availability of forms with far superior absorption. [17] It has previously been suggested that individual variability in blood level response to a common dose of 1g could leave a substantial number of patients at an increased risk of CVD, simply due to failure to achieve a therapeutic EPA + DHA level of between 8-10%. For example, while an omega-3 dose of 1g daily (as ethyl-ester) has been shown to increase the Omega-3 Index from a mean of 3.6% to 5.4%, approximately 16% of the study participants achieved an EPA + DHA blood level less than 4.8% and this is clinically relevant since it has been noted that an omega-3 index >5 % is the range in which dramatic reduction in sudden coronary death can be observed. [18] It is also important to acknowledge that the Omega-3 Index is influenced by many factors, such as smoking, age, sex, body weight, physical activity and genes, yet intra-individual variation in response to omega-3 intake is rarely acknowledged. While omega-3s faced some criticism in the area of cardiovascular health, 2018 reported some very encouraging outcomes in other areas of health, most notably, pregnancy, liver and mood!
Omega-3 and pregnancy
Pregnancy creates a ‘natural’ state of heightened oxidative stress and inflammation. Maternal intake of omega-3 and omega-6 fats can strongly influence placental growth and levels of inflammation & oxidative stress. Dietary intake of fats can, therefore, have subsequent effects on the risk of developing pregnancy complications and on infant health, with increased omega-3 intake both before and during pregnancy known to offer significant benefits. Indeed, a Cochrane review of 70 randomised trials found that increasing omega-3 intake at 12-weeks of pregnancy reduced the risk of having a premature baby (<37 weeks) by 11%, the risk of having an early premature baby (<34 weeks) by 4% and the risk of having a small baby (less than 2500g) by 10%. [19] The ideal dose for achieving optimal outcomes appears, however, to vary between individuals, and while many women do supplement during pregnancy, it is likely that many do not consume adequate amounts of EPA & DHA or at the optimal ratio, to provide protection against pregnancy complications such as preterm birth (~ 1g per day of which 500mg suggested as DHA). It is also important to acknowledge the potential for adverse effects (increased oxidative stress) from very high doses of DHA alone (without EPA) as the mother-to-be reaches term, because the preterm placenta is significantly more sensitive to oxidative damage. In addition, because DHA supplementation during pregnancy (as shown by the DOMinO dietary intervention study) leads to high variation in cord blood DHA levels at delivery, not only does the optimal dose vary between individuals [20], but the absence of EPA may have adverse consequences. It is not uncommon for pregnancy products to focus on DHA (with many providing pure DHA only), and because the retro-conversion of DHA to EPA in pregnant women is only around 4–11% when supplementing with a pure DHA supplement, this could leave them with an EPA insufficiency that may indirectly promote inflammation. The omega-6 fatty acid arachidonic acid (AA) is the precursor of the potent 2-series prostaglandins (PGE2 and PGF2) associated with the initiation of labour and preterm labour and the vasoconstrictor thromboxane (TXA2) associated with pre-eclampsia. Unlike DHA, which is not involved with eicosanoid formation, EPA is the precursor for the 3-series of prostaglandins PGE3 and PGI3, which promote relaxation of the uterine wall. Not only does EPA produce less inflammatory prostaglandins, but it also competitively displaces AA in cell membranes, thereby reducing the production of 2-series eicosanoids. A high ratio of AA to EPA may act to fuel the heightened oxidative stress and inflammation that exists during pregnancy while also promoting a higher risk of developing pregnancy complications. In addition, EPA mediates DHA’s transfer across the placenta and its transport and uptake into foetal cells. As such, including EPA in equal parts or slightly higher than that of DHA will not only support DHA accumulation but, by optimising a healthy AA to EPA ratio (<3), can also ensure an environment that favours healthy pregnancy outcomes. [21]
Liver health
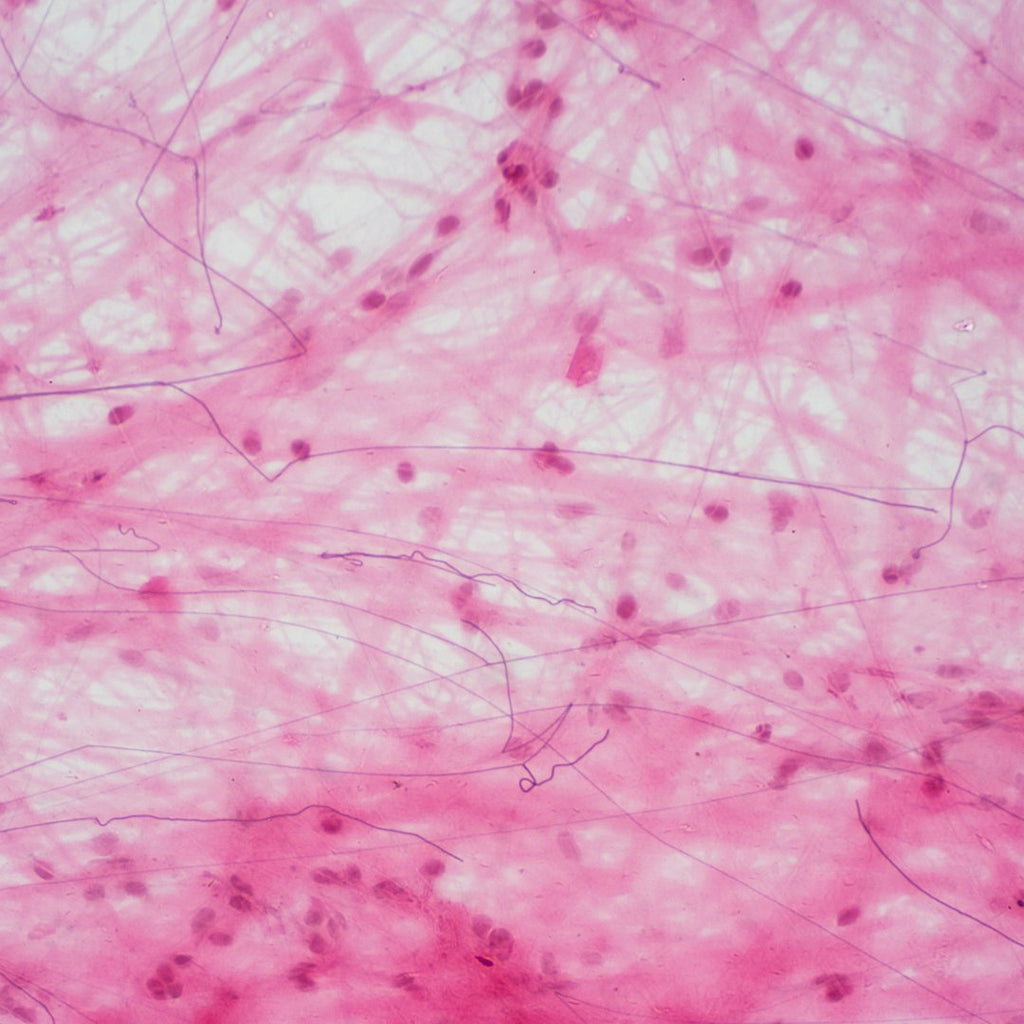
Omega-3s act to prevent chronic low-grade inflammation by inhibiting inflammatory cytokines (such as TNF-α IL-1 and IL-6) and proinflammatory eicosanoids (such as thromboxane-2 and prostaglandin E2). [22] As the omega-3 index is inversely related to biomarkers of inflammation (including CRP, cytokines & eicosanoids), maintaining an Omega-3 Index ≥8% can help regulate a healthy inflammatory balance, improve inflammation symptoms and possibly reduce the progression and severity of inflammatory-related conditions. [23] Individuals with alcoholic liver disease (ALD) and non-alcoholic fatty liver disease (NAFLD) present with high levels of hepatic saturated & monounsaturated fat and low omega-3, a characteristic associated with hepatic lipotoxicity, inflammation, oxidative stress and fibrosis. [24] Studies published in 2018 support the use of EPA & DHA to protect against liver injury (both ALD and NAFLD), suggesting that supplementation with omega-3 may offer a natural approach to managing these common diseases via anti-inflammatory mechanisms and by reducing oxidative stress and storage by the liver. [25, 26]
Mood disorders
Inflammation is a key mechanism in the pathophysiology of mood disorders, including major depression, post-natal depression, bipolar disorder, and post-traumatic stress disorder (PTSD). As eicosanoids are essential for brain function and regulating the inflammatory response, it is not surprising that low omega-3 status or an imbalance between levels of AA and EPA can create a pro-inflammatory environment that predisposes an individual to mental health issues or drives pre-existing illness duration and severity. [27] Clinical trials using DHA and/or EPA show promising results on depressive symptoms that appear to be related to the effects of EPA on inflammation. Patients with higher inflammatory markers (such as CRP and cytokines) experience greater improvement in mood symptoms in response to EPA, but not DHA, and those individuals with the lowest baseline levels of omega-3 are more likely to benefit from supplementation than individuals with higher levels. [28, 29] Similar to results from cardiovascular studies, not all dietary interventions using omega-3 to modify mood report positive outcomes. Polokowski’s systematic review of omega-3 in the treatment of anxiety disorders highlighted that very few study designs meet the acceptance criteria and that if omega-3 fatty acids are going to be utilised as a therapeutic option, then it is imperative to address the current and repeated flaws in study designs that hinder successful outcomes. The discrepancies reported (in both mood and cardiovascular interventions) are often explained by the lack of standardisation including the inclusion criteria used, the EPA to DHA ratio and dose, the ability of a supplement regime to increase omega-3 status, the omega-3 baseline status of subjects, and the methods of diagnosis used to identify potential responders. [29, 30]
Summary
The consequences of omega-3 deficiency affect most body organs, with most chronic disease directly linked to low omega-3 status. The effects of EPA and DHA on health outcomes are clearly influenced by baseline levels and the benefits are most likely dose-dependent, yet these key ‘influencers’ are often not taken into account either during study design or in the interpretation of study outcomes. The Omega-3 Index is a powerful biomarker that can be applied universally to ensure that supplementation (whether in large-scale studies or on an individual basis) fulfills the purpose of increasing omega-3 status – to reduce the risk of chronic disease. With the average intake of omega-3 unlikely to achieve levels known to reduce risk, it is important that the public is made aware of not just how essential omega-3s are to our health but, more so, the consequences that can arise when levels fall low. In part two of our Omega-3 research update series, we discuss the value of testing and how to use the Omega-3 Index to make improvements to long-term health.
References
- Calder PC. Mechanisms of action of (n-3) fatty acids. J Nutr. 2012 Mar;142(3):592S-599S.
- Calder PC. Very long-chain n-3 fatty acids and human health: fact, fiction and the future. Proc Nutr Soc. 2018 Feb;77(1):52-72.
- Abdelhamid AS, Brown TJ, Brainard JS, Biswas P, Thorpe GC, Moore HJ, Deane KH, AlAbdulghafoor FK, Summerbell CD, Worthington HV, Song F, Hooper L. Omega-3 fatty acids for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev. 2018 Jul 18;7:CD003177.
- Aung T, Halsey J, Kromhout D, et al. Associations of omega-3 fatty acid supplement use with cardiovascular disease risks. Meta-analysis of 10 trials involving 77,917 individuals. JAMA Cardiology. 2018;3(3):225-234.
- Maki KC. Long-Chain Omega-3 Fatty Acid Bioavailability: Implications for Understanding the Effects of Supplementation on Heart Disease Risk. J Nutr. 2018 Nov 1;148(11):1701-1703.
- Tribulova N, Szeiffova Bacova B, Egan Benova T, Knezl V, Barancik M, Slezak J. Omega-3 Index and Anti-Arrhythmic Potential of Omega-3 PUFAs. Nutrients. 2017 Oct 30;9(11). pii: E1191. doi: 10.3390/nu9111191. Review.
- Harris WS, Tintle NL, Etherton MR, Vasan RS. Erythrocyte long-chain omega-3 fatty acid levels are inversely associated with mortality and with incident cardiovascular disease: The Framingham Heart Study. J Clin Lipidol. 2018 May – Jun;12(3):718-727.
- Dyerberg J, Madsen P, Møller JM, Aardestrup I, Schmidt EB. Bioavailability of marine n-3 fatty acid formulations. Prostaglandins Leukot Essent Fatty Acids. 2010 Sep;83(3):137-41.
- Flock, M. R., A. C. Skulas-Ray, et al. (2013). “Determinants of erythrocyte omega-3 fatty acid content in response to fish oil supplementation: a dose-response randomized controlled trial.” J Am Heart Assoc 2(6): e000513.
- Kromhout D, Giltay EJ, Geleijnse JM; Alpha Omega Trial Group. n-3 fatty acids and cardiovascular events after myocardial infarction. N Engl J Med. 2010 Nov 18;363(21):2015-26
- Rauch B, Schiele R, Schneider S, Diller F, Victor N, Gohlke H, Gottwik M, Steinbeck G, Del Castillo U, Sack R, Worth H, Katus H, Spitzer W, Sabin G, Senges J; OMEGA Study Group. OMEGA, a randomized, placebo-controlled trial to test the effect of highly purified omega-3 fatty acids on top of modern guideline-adjusted therapy after myocardial infarction. Circulation. 2010 Nov 23;122(21):2152-9.
- Galan P, Kesse-Guyot E, Czernichow S, Briancon S, Blacher J, Hercberg S; SU.FOL.OM3 Collaborative Group. Effects of B vitamins and omega 3 fatty acids on cardiovascular diseases: a randomised placebo controlled trial. BMJ. 2010 Nov 29;341:c6273. doi: 10.1136/bmj.c6273.
- ORIGIN Trial Investigators, Bosch J, Gerstein HC, Dagenais GR, et al. n-3 fatty acids and cardiovascular outcomes in patients with dysglycemia. N Engl J Med. 2012;367(4):309-318
- Risk and Prevention Study Collaborative Group, Roncaglioni MC, Tombesi M, Avanzini F, Barlera S, Caimi V, et al. N-3 fatty acids in patients with multiple cardiovascular risk factors. New England Journal of Medicine 2013;368(19):1800–8
- Bowman L, Mafham M, Stevens W, Haynes R, Aung T, Chen F, Buck G, Collins R, Armitage J; ASCEND Study Collaborative Group. ASCEND: A Study of Cardiovascular Events iN Diabetes: Characteristics of a randomized trial of aspirin and of omega-3 fatty acid supplementation in 15,480 people with diabetes. Am Heart J. 2018 Apr;198:135-144.
- Manson J.E., Cook N.R., Lee I.M., Christen W., Bassuk S.S., Mora S., Gibson H., Albert C.M., Gordon D., Copeland T., et al. Marine n− 3 fatty acids and prevention of cardiovascular disease and cancer. N. Engl. J. Med. 2018 doi: 10.1056/NEJMoa1811403
- Maki KC, Dicklin MR. Strategies to improve bioavailability of omega-3 fatty acids from ethyl ester concentrates. Curr Opin Clin Nutr Metab Care. 2018 Dec 12.
- Rupp H, Wagner D, Rupp T, Schulte LM, Maisch B.Risk stratification by the “EPA+DHA level” and the “EPA/AA ratio” focus on anti-inflammatory and antiarrhythmogenic effects of long-chain omega-3 fatty acids. Herz. 2004 Nov;29(7):673-85. Review.
- Middleton P, Gomersall JC, Gould JF, Shepherd E, Olsen SF, Makrides M. Omega-3 fatty acid addition during pregnancy. Cochrane Database of Systematic Reviews 2018, Issue 11 . Art. No.: CD003402. DOI:
- Muhlhausler BS, Gibson RA, Yelland LN, Makrides M. Heterogeneity in cord blood DHA concentration: towards an explanation. Prostaglandins Leukot Essent Fatty Acids. 2014 Oct;91(4):135-40.
- Büyükuslu N, Ovalı S, Altuntaş ŞL, Batırel S, Yiğit P, Garipağaoğlu M. Supplementation of docosahexaenoic acid (DHA) / Eicosapentaenoic acid (EPA) in a ratio of 1/1.3 during the last trimester of pregnancy results in EPA accumulation in cord blood. Prostaglandins Leukot Essent Fatty Acids. 2017 Oct;125:32-36
- Li K, Huang T, Zheng J, Wu K, Li D. Effect of marine-derived n-3 polyunsaturated fatty acids on C-reactive protein, interleukin 6and tumor necrosis factor α: a meta-analysis. PLoS One. 2014 Feb 5;9(2):e88103.
- Rangel-Huerta OD, Aguilera CM, Mesa MD, et al. Omega-3 long-chain polyunsaturated fatty acids supplementation on inflammatory biomarkers: a systematic review of randomised clinical trials. Br J Nutr2012;107 S159–70.
- Spooner MH, Jump DB. Omega-3 fatty acids and nonalcoholic fatty liver disease in adults and children: where do we stand? Curr Opin Clin Nutr Metab Care. 2019 Mar;22(2):103-110.
- Wang M, Ma LJ, Yang Y, Xiao Z, Wan JB.n-3 Polyunsaturated fatty acids for the management of alcoholic liver disease: A critical review. Crit Rev Food Sci Nutr. 2018 Dec 22:1-14.
- Musa-Veloso K, Venditti C, Lee HY, Darch M, Floyd S, West S, Simon R.Systematic review and meta-analysis of controlled intervention studies on the effectiveness of long-chain omega-3 fatty acids in patients with nonalcoholic fatty liver disease. Nutr Rev. 2018 Aug 1;76(8):581-602. doi: 10.1093/nutrit/nuy022.
- Scola G, Versace A, Metherel AH, Monsalve-Castro LA, Phillips ML, Bazinet RP, Andreazza AC. Alterations in peripheral fatty acid composition in bipolar and unipolar depression. J Affect Disord. 2018 Jun;233:86-91
- Carney RM, Steinmeyer BC, Freedland KE, Rubin EH, Rich MW, Harris WS. Baseline blood levels of omega-3 and depression remission: a secondary analysis of data from a placebo-controlled trial of omega-3 supplements. J Clin Psychiatry. 2016 Feb;77(2):e138-43.
- Larrieu T, Layé S. Food for Mood: Relevance of Nutritional Omega-3 Fatty Acids for Depression and Anxiety. Front Physiol. 2018 Aug 6;9:104
- Polokowski AR, Shakil H, Carmichael CL, Reigada LC. Omega-3 fatty acids and anxiety: A systematic review of the possible mechanisms at play. Nutr Neurosci. 2018 Sep 28:1-11.