With magnesium supplements commonplace on practitioners’ shelves, how can we be sure that the product we recommend will offer the most effective solution to optimising both uptake and retention of a client’s magnesium levels?
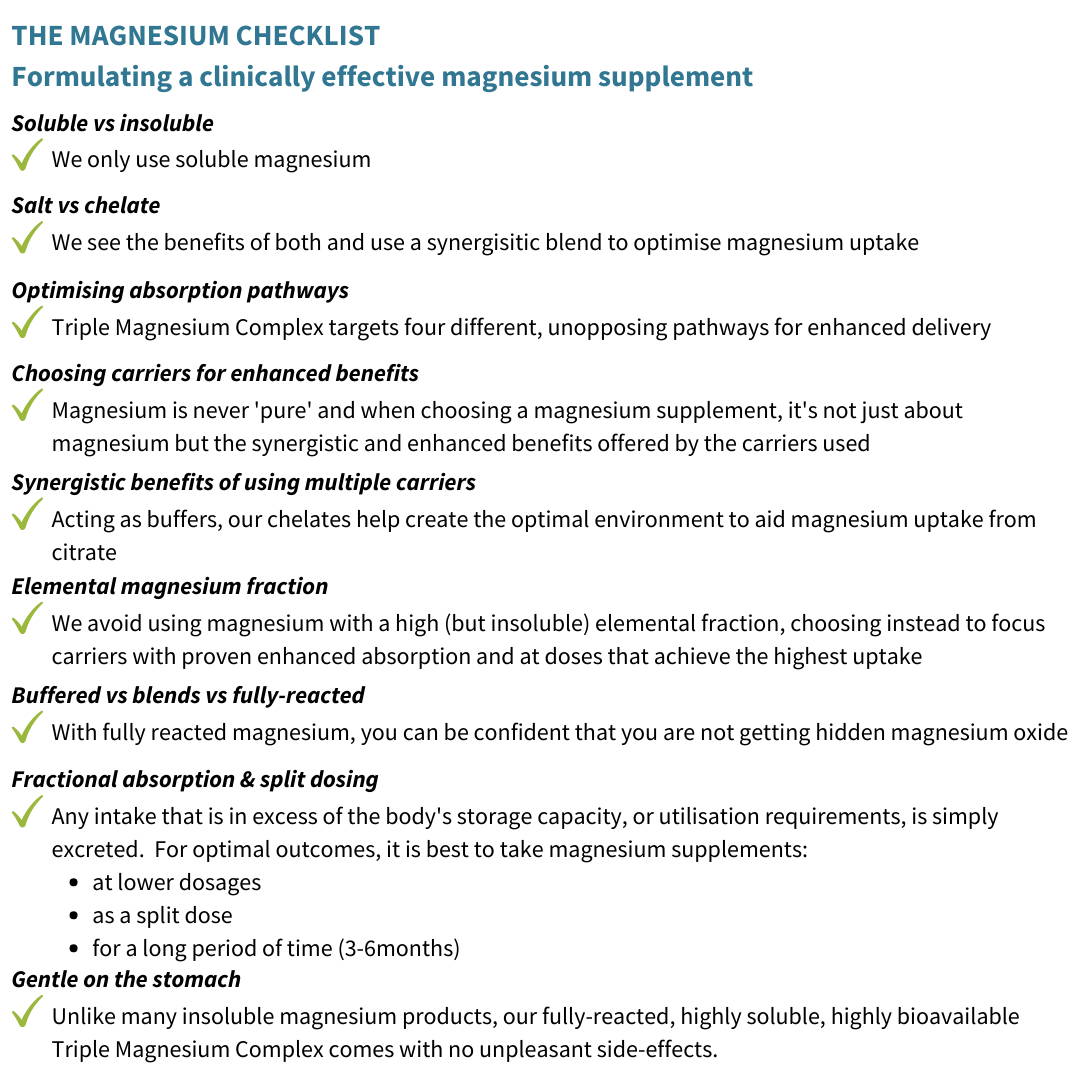
September sees the launch of our new ‘Triple Magnesium Complex’, a trio of citrate, bisglycinate and taurate, all in their ‘fully reacted’ forms (not ‘blended’ or ‘buffered’, meaning there’s no added magnesium oxide to artificially boost elemental label claims), ‘chelated’ (bonded) synergistically to target multiple absorption pathways with no risk of unpleasant gastrointestinal (GI) side effects.
Before Triple Magnesium Complex is quickly dismissed as yet another magnesium supplement, let us discuss the perils and pitfalls uncovered during R&D that drove our passion to provide a clinically superior alternative, making Triple Magnesium Complex the only magnesium supplement that should be on your dispensing shelf! In this article we aim to help you navigate the complex nature of magnesium supplementation, dose and absorption, and also explain the many factors that will affect the efficacy of your favoured product.
Magnesium: ‘ A review of the basics’:
- A huge 60% of the population are not meeting a daily adequate intake of 300mg magnesium
- Magnesium is the second most abundant mineral in the body after potassium, with a healthy adult human body estimated to contain approximately 24.4g of magnesium (based on a 70kg individual)
- Normal total serum magnesium concentration of a healthy individual is in the range of 0.7–1.1 mmol/l (or between 1.65 and 2.52 mmol/l when testing red blood cells). In order to maintain these levels, a minimum daily magnesium intake of about 3.6 mg/kg is necessary (~252mg for a 70kg person)
- The majority of magnesium is stored in the bones, muscles and soft tissues, with around 30% of bone stores functioning as an easily accessible reservoir for ‘topping-up’ levels when magnesium intake is low
- Prolonged deficiency in magnesium can result in bones being ‘leached’ of magnesium reserves, in turn compromising healthy bones (1)
- While the absorption of magnesium varies depending on how much magnesium the body needs, studies consistently show us that when magnesium is taken in small doses throughout the day, it is taken up and retained more effectively than a single high dose which may actually lead to loose stools and diarrhoea
- Serum levels of magnesium are tightly regulated by a carefully orchestrated balance of absorption (via the gut) and excretion (via the kidney), with excess magnesium (over 24.4g normal capacity for reserves) unable to be stored and therefore excreted by the kidneys
The consequences of magnesium deficiency
Magnesium plays a critical role in nerve transmission, cardiac excitability, neuromuscular conduction, muscular contraction, vasomotor tone, blood pressure, and glucose and insulin metabolism and plays a major role in both disease prevention and overall health. Deficiency of magnesium is linked to various disorders including cardiovascular (congestive heart failure, arrhythmia, myocardial infarction, stroke, hypertension) skeletal/muscular (muscle spasms & cramps e.g. restless leg syndrome), gastrointestinal tract (constipation), metabolic and central nervous system (irritability, anxiety, lethargy, impaired memory & cognitive function), contributing to depression, chronic fatigue syndrome, epilepsy, preeclampsia, Parkinson’s disease, sleeping problems, headache, osteoporosis, cardiovascular disease, metabolic syndrome and type II diabetes (2, 3, 4 & 5). Conversely, a beneficial effect of magnesium supplementation has been observed for most of these diseases/conditions (Table 1).
Table 1: Health conditions and diseases associated with low magnesium status for which magnesium therapy is, or may be, beneficial [adapted from 6 & 7].
The good news is magnesium supplements are a convenient way of overcoming magnesium deficiencies; however, there are many factors to consider when choosing a magnesium supplement that provides clinical efficacy. Whilst most practitioners are knowledgeable about the different forms magnesium may come in, many favourable forms of magnesium (citrate, bisglycinate, malate and so on) may still contain hidden magnesium oxide, the least preferred form, well known for its laxative effect and poor bioavailability. Let’s consider the points that will help you identify if your ‘go-to’ magnesium citrate, is really providing a magnesium reacted to citrate to offer superior absorption over magnesium oxide, or if it’s simply a magnesium oxide with added citrate, therefore not providing the benefits it promises.
Choosing the most bioavailable magnesium supplement
There are a number of magnesium supplements offering a range of bioavailability and health benefits. As we know, there are many factors to consider when choosing a supplement, which is why it’s easy to ‘stick to what we know’. When considering what makes a ‘good’ magnesium, the following factors should be considered because they have a direct influence on the efficacy of a magnesium supplement.
1. Elemental vs fractional magnesium – what does this mean to the bioavailability of a magnesium supplement?
Magnesium supplements are never ‘pure’, with the elemental magnesium fraction of a supplement ranging from as little as 6% up to 60%. It is understandable, therefore, to assume that products with a higher elemental fraction delivering a high dose of elemental magnesium, with minimum capsules/tablets, would be the better choice. As practitioners, though, we know that it’s not all about how much we take, but more about how much we absorb. When it comes to magnesium, it’s crucial to be aware that supplements with the highest elemental fraction are generally poorly absorbed. Magnesium oxide, for example, has the highest magnesium elemental concentration (60%), but as it is one of the least soluble of all magnesium forms it has very low bioavailability (estimated at 4% of the elemental fraction). In contrast, magnesium citrate provides 12% elemental magnesium and has one of the highest absorption rates at around 25%, especially when taken at low doses (we will discuss the benefits of split dosing later!).
As we know, the cheaper forms of magnesium supplements contain magnesium oxide, as its higher elemental fraction provides an easy marketing tool to boost label claims, with a supplement apparently delivering the full RI (375mg) in just 625mg total; however, at an absorption rate of just 4%, the amount of magnesium delivered is a pitiful 15mg! So what do we mean by solubility and how does this affect the bioavailability of magnesium?
While we know that the fractional amount of magnesium is important, the bioavailability of other forms of magnesium are much preferable (even though they may still contain hidden magnesium oxide…we’ll get to that bit).
2. Forms of magnesium – the importance of solubility and chelates in improving magnesium bioavailability
Table 2: Health conditions and diseases associated with low magnesium status for which magnesium therapy is, or may be, beneficial [adapted from 6 & 7].
Solubility – if the magnesium is insoluble, it cannot be absorbed
Whilst many are familiar with the concept that magnesium oxide is insoluble, here is a quick summary to detail how this affects the efficacy of an oxide-containing supplement.
Magnesium from magnesium salts (such as oxide, sulfate, hydroxide, chloride or citrate) is absorbed only after the magnesium is liberated from its salt. Solubility therefore refers to the ease with which a magnesium salt releases its magnesium ion and is one of the most influential factors affecting bioavailability.
Insoluble magnesiums (oxide, carbonate & hydroxide) require an acid environment to break the bond between the salt and the magnesium. In contrast, soluble salts such as citrate do not require the presence of acid to release their magnesium ion. Thus, citrate has an immediate advantage over the insoluble salts, because insoluble salts will remain unabsorbable unless the environment is favourable enough to break this bond between the salt and the magnesium. Once magnesium has been freed from its carrier, the majority will be absorbed via paracellular ion absorption pathways, (where magnesium moves between the tight junctions of the GI tract). This is important when we consider clients with high levels of stress, which magnesium supplements are often used to support, as low stomach acid levels often follow.
Chelates – an amino acid carrier with exceptional bioavailability and benefits
In contrast to magnesium salts, magnesium ‘chelates’, such as glycinate and taurinate, bypass ion channels and are instead absorbed in the same way that amino acids are absorbed from the diet. They can do this because the bond that joins magnesium to an amino acid is incredibly strong and works in favour of magnesium absorption because as the amino acid crosses the cell membrane, it pulls magnesium in after itself, essentially giving magnesium a free ride. The benefit of the chelate doesn’t end there. When considering the absorption of a magnesium salt, when the magnesium ion is liberated from the salt, unless it is immediately absorbed by an ion channel it remains extremely vulnerable, attracting water and becoming too big to be absorbed, or forming bonds with compounds found in food (oxalates and phytates) and becoming insoluble.
Unlike magnesium salts, the strong bond that exists between magnesium and its amino acid carrier minimises the accumulation of ‘free’ highly reactive, unstable ions. By not liberating magnesium, chelates prevent the formation of insoluble compounds that a salt would allow, thereby making them superior to salts.
Choosing between a magnesium salt and a magnesium chelate
As you can see, there are benefits to both magnesium salts and magnesium chelates in terms of bioavailability. By combining magnesium citrate, as a soluble salt, and magnesium bisglycinate and taurinate, as chelates, Triple Magnesium Complex is able to benefit from multiple unopposing absorption pathways – four, to be exact. Furthermore, these three forms of magnesium create a favourable acidic environment to protect free magnesium ions from interacting with food or water that would, under normal circumstances, interfere with magnesium uptake, and thus enhancing the absorption of free ions.
3. Finding the hidden oxide in your ‘superior’ magnesium supplement – the importance of ‘fully-reacted’
Magnesium can come with one of three features: as a blend, a buffer or a fully reacted supplement. Whilst many practitioners are aware that a blend contains magnesium oxide, did you know that a buffered magnesium supplement also contains magnesium oxide? So, whilst a product may have a label claim of magnesium citrate, magnesium bisglycinate or magnesium taurate, unless it clearly states that the product contains fullyreacted magnesium, much of your elemental claim will come from magnesium oxide.
Understanding the difference:
Magnesium ‘blends’ simply blend magnesium oxide with a carrier such as citrate. No reaction takes place, the elemental magnesium is 100% insoluble magnesium oxide, with citrate only added to lower the pH to favour the release of the magnesium ions.
If you are taking a magnesium product and experiencing gastrointestinal upset, the chances are it will be a blended product with high oxide content. In contrast, fully reacted magnesium forms complexes and are directly bound to the carrier via a manufacturing process, therefore containing no magnesium oxide and the total elemental magnesium is 100% soluble magnesium citrate.
‘Buffered’ products combine fully reacted magnesium (such as fully reacted magnesium citrate) with magnesium oxide. This is usually done to boost the elemental magnesium label claim. While buffers are superior to blends in terms of delivering soluble bioavailable magnesium, they still deliver an unknown fraction of insoluble magnesium oxide. The higher the elemental magnesium, the more oxide it likely contains.
Fully reacted magnesium is superior to buffered magnesium supplements or blends which contain magnesium oxide
Our Triple Magnesium Complex of citrate, bisglycinate and taurate delivers 100% fully-reacted magnesium, so that practitioners can be confident they are recommending the most soluble, bioavailable forms of magnesium possible, with no risk of unpleasant side-effects.
Did you know? The laxative side effect experienced with magnesium oxide occurs as a result of the movement of water out of the mucosa cell and into the gut lumen in an attempt to equalise the concentration of magnesium between the two environments (osmosis).
4. The importance of dose – a formulation to maximise intake in the body
Studies have shown that the absorption of magnesium from a low elemental dose can be as high as 65% and that when the dose exceeds 250mg, the relative absorption is reduced to as little as 21%. (Fine et al 1991). It therefore makes sense to optimise the absorption and retention of magnesium by splitting our Triple Magnesium Complex daily dose into 2 smaller doses (131mg each). This carefully considered dose focuses on retention rather than excretion. As previously discussed, the body carefully regulates plasma magnesium levels, with excess intake above the body’s capacity to handle, simply resulting in magnesium loss. Our ethos is to focus on the efficacy of delivery, using three of the most absorbable and synergistic ‘carriers’ to target multiple, unopposed uptake pathways with the emphasis on split-dosing to optimise both absorption and retention.
Study 1: Graham LA, Caesar JJ & Burgen ASV (1960) Gastrointestinal absorption and excretion of Mg-28 in man. Metabolism-Clinical and Experimental 9, 646-659. Study 2: Roth P & Werner E (1979) Intestinal absorption of magnesium in man. International Journal of Applied Radiation and Isotopes 30, 523-526. Study 3: Fine KD, Santa Ana CA, Porter JL, Fordtran JS. Intestinal absorption of magnesium from food and supplements. J Clin Invest. 1991 Aug;88(2):396-402.
Let’s not forget – magnesium absorption takes place in the small intestine, with the absorption capacity influenced by the length of that intestinal segment, transit time, mucosal integrity, pH of the lumen, rate of gastric emptying, the size of meal and the use of motility and antimotility drugs. With this in mind, compared with formulations that overwhelm the body’s ability to absorb and retain magnesium, a supplement that offers a slow, sustained exposure to magnesium throughout the day will help optimise magnesium uptake more efficiently.
When considering magnesium supplementation, an individual’s current magnesium status is the primary influencer of how much magnesium is absorbed and retained. Therefore, higher doses may become appropriate when you have results to confirm blood levels are low, as absorption will be higher and less will be excreted.
5. Getting the best from your magnesium: choose your carrier wisely
Many practitioners select a magnesium supplement based on the added benefits of the carrier; citrate, for example, supports energy production, taurine supports insulin sensitivity and so on. By combining three forms, individual clients can benefit from every feature, negating the need for several supplements.
A brief summary of the added benefits of magnesium carriers
Glycine is involved in collagen formation, creatine formation, glutathione production and haemoglobin production, whilst also acting as an inhibitory neurotransmitter. The two glycine molecules in magnesium bisglycinate occupy the reactive sites of magnesium, preventing it from forming insoluble complexes (with phytates & oxalates), thereby helping to increase uptake and retention of magnesium. Taurine acts as an antioxidant and helps improve insulin sensitivity but is possibly best known for its cardiovascular benefits and for its positive influence on bone metabolism. In addition, taurine & glycine are highly effective carriers that, by acting as pH buffers, help create the optimal environment to aid magnesium uptake from citrate, allowing citrate to then feed into the citric acid (Krebs) cycle to help support energy.
Other factors affecting magnesium status
Whilst choosing the best quality supplements is paramount for effectiveness, it is also important to acknowledge factors affecting an individual’s magnesium levels.
People who live on a diet that is high in refined and processed carbohydrates are at a higher risk of insufficiency/deficiency; this is becoming worryingly common and can have a significant negative impact on our health.
In addition, common drugs that interfere with magnesium absorption (such as H2 antihistamines and proton pump inhibitors) or enhance excretion either via the GI tract (such as laxatives) or by renal loss (such as diuretics) are all known to contribute to the low magnesium status of the UK population. It is also not uncommon for individuals with pre-existing health conditions that negatively affect magnesium status (such as diabetes, osteoporosis, heart disease, GI disorders & renal disease) to further compromise magnesium status by taking drugs that interfere with magnesium absorption and retention.
Summary
With rates of magnesium deficiency already high and on the increase, and the benefits of magnesium supplements well established, it is clearly a priority to choose the most effective magnesium product for use in clinical practice, in order to have the greatest impact on improved health. Triple Magnesium Complex is the latest addition to our clinical range of nutraceutical products, and we are confident it is the most clinically effective magnesium product available to practitioners.
References:
- Jahnen-Dechent W, Ketteler M. Magnesiumbasics. Clin Kidney J. 2012 Feb;5(Suppl 1):i3-i14.
- Eby GA, Eby KL. Rapid recovery from major depression using magnesium treatment. Med Hypotheses. 2006;67(2):362-70.
- Volpe SL. Magnesium in disease prevention and overall health. Adv Nutr. 2013 May 1;4(3):378S-83S. doi: 10.3945/an.112.003483. Review.
- Gums JG. Magnesium in cardiovascular and other disorders. Am J Health Syst Pharm. 2004 Aug 1;61(15):1569-76. Review.
- Tong GM, Rude RK. Magnesium deficiency in critical illness. J Intensive Care Med. 2005 Jan-Feb;20(1):3-17. Review.
- de Baaij JH, Hoenderop JG, Bindels RJ Magnesium in man: implications for health and disease. Physiol Rev. 2015 Jan;95(1):1-46
- Geiger H, Wanner C. Magnesium in disease. Clin Kidney J. 2012 Feb;5(Suppl 1):i25-i38.
- National Diet and Nutrition Survey. Results from Years 5-6 (combined) of the Rolling Programme (2012/13 – 2013/14)
- Buttriss J. Nutrient requirements and optimisation of intakes. Br Med Bull. 2000;56(1):18-33. Review.
- Uwitonze AM, Razzaque MS. Role of Magnesium in Vitamin D Activation and Function. J Am Osteopath Assoc. 2018 Mar 1;118(3):181-189
- Coudray C, Rambeau M, Feillet-Coudray C, Gueux E, Tressol JC, Mazur A, Rayssiguier Y. Study of magnesium bioavailability from ten organic and inorganic Mg salts in Mg-depleted rats using a stable isotope approach. Magnes Res. 2005 Dec;18(4):215-23.
- Schuette SA, Lashner BA, Janghorbani M Bioavailability of magnesium diglycinate vs magnesium oxide in patients with ileal resection. JPEN J Parenter Enteral Nutr. 1994 Sep-Oct;18(5):430-5.
- Graham LA, Caesar JJ & Burgen ASV (1960) Gastrointestinal absorption and excretion of Mg-28 in man. Metabolism-Clinical and Experimental 9, 646-659.
- Roth P & Werner E (1979) Intestinal absorption of magnesium in man. International Journal of Applied Radiation and Isotopes 30, 523-526.
- Fine KD, Santa Ana CA, Porter JL, Fordtran JS. Intestinal absorption of magnesium from food and supplements. J Clin Invest. 1991 Aug;88(2):396-402.