The occasional bout of bloating or feeling too full after a big meal is considered normal, but if your bloating is unbearable on a day-to-day basis and is accompanied by pain and cramping, it’s time to do some investigation work to see what your digestive issues are.

Feeling the bloat after a large meal is often due to undigested food particles fermenting in the gut, producing excess gases which accumulate in your large intestine.
Figuring out which foods make you bloat, optimising digestion, balancing gut flora and maintaining a healthy gut lining can go a long way in helping to control symptoms of bloating and painful cramping.
BLOATING AND UNDIGESTED FOOD
If your ability to break down food is compromised, you will most likely end up with undigested food particles in your large intestine, the perfect feeding ground for certain types of bacteria producing gas. When this occurs, you will most likely experience bloating.
The process of breaking down food starts the moment we chew our food: the mouth releases saliva containing amylase, a digestive enzyme to begin the process of digestion while we chew food into smaller pieces. This enzyme production is even stimulated by the smell of a tasty meal cooking, preparing the digestive system for what is to come. In the stomach, hydrochloric acid is then released to break food into even smaller particles. The stomach, pancreas and small intestines complete the digestion process by releasing a host of powerful digestive enzymes to further break down food, ready for the absorption of nutrients.
If the digestion process is hindered on a regular basis, undigested food particles may pass into the intestines and the immune system may eventually react to them, resulting in a food intolerance. Additional inflammation associated with food intolerances may also result in excess bloating and cramping.
One of the simplest ways to give your digestion a chance to break down food and reduce bloating is to chew your food properly. Chewing food to a pulp until no lumps are left and allowing saliva to start the digestion process can give your digestive system a substantial break. Remember, our intestines don’t have teeth! Additionally, taking time to prepare for meals and paying attention to the smell of your food should help support the production of digestive enzymes and stomach acid.
If these simple steps don’t provide relief of your symptoms, you may wish to take a supplement to increase your levels of digestive enzymes to help break down your food. Digestive enzymes combined with betaine hydrochloride (HCl) can also help to support stomach acid levels. Taking HCl is particularly helpful if you find it difficult to digest large protein-rich meals, or if you experience reflux or prolonged fullness after a meal. A broad-spectrum digestive enzyme supplement is ideal to ensure each stage of the digestion process is supported, and to aid in the breakdown of a wide range of foods.

FOODS TO REDUCE BLOATING
While our ability to break down foods in general can make a huge difference to how much we bloat, there are some foods which are more problematic than others, and which foods make you bloat may vary from person to person.
Milk, for example, may be easy for some to digest but difficult for others. The variation in our ability to digest certain foods depends on the enzymes we produce. When someone lacking the digestive enzyme lactase (required to break down lactose - the natural sugar in milk) consumes foods containing lactose, they experience an increased production of gas. (1)
Which foods make you bloat often corresponds to difficulties digesting different types of carbohydrates. The main group of commonly aggravating carbohydrates includes ‘FODMAPs’, a group of short-chain carbohydrates including fructose (found in fruit), lactose (found in milk), sugar alcohols such as xylitol (often found in chewing gum) and other foods such as onions, garlic, beetroot, beans, peas and wheat. You can read more about FODMAPs here.
Following a low FODMAP diet, i.e. limiting foods such as fruit, milk and wheat, has shown to be very effective at reducing bloating. (2) When specifically looking at the effects of fructose, for example, low absorption and fermentation of fructose causes gas production, while restriction of high-fructose foods has been shown to reduce symptoms of bloating. (3, 4)
Fibre-rich foods also commonly cause bloating and flatulence symptoms, such as wheat, barley and rye, fruit and beans. (5) These difficult to digest foods require a good production of digestive enzymes amylase and cellulase, therefore if levels are low, undigested food is likely to ferment in the gut. Fibre-rich foods also absorb a lot of water, producing a significant amount of bulk in your digestive tract. An individual’s sensitivity to gases produced by fermentable fibres can vary greatly from person to person, and bacteria present in the gut can also affect tolerability of such gases.
To help reduce bloating, try taking a digestive enzyme supplement containing amylase and cellulase to aid the breakdown of fibre and plant cellulose. If symptoms persist, you may then wish to consider temporarily cutting out the common culprits, including gluten, beans and lentils, to find out which foods make you bloat. If your digestive system is healthy with a good production of digestive enzymes, balanced gut bacteria and a good gut lining integrity, you should be able to digest these foods reasonably well without too much bloating.
REDUCE BLOATING BY BALANCING BACTERIA IN THE GUT
If a bacterial imbalance, often referred to as dysbiosis, is to blame for your bloating, probiotics may help to ease your symptoms. A healthy balance of bacteria and yeast actually supports digestion in the large intestine, whereas pathogenic ‘bad’ bacteria may be feeding off your food and expelling gases as their waste products.
Placebo-controlled trials have shown that supplementing with probiotics does help to reduce bloating in individuals with irritable bowel syndrome (IBS) and also for those who simply experience bloating. (6)
Taking a multi-strain probiotic supplement is ideal for anyone experiencing bloating symptoms, but be wary of probiotic drinks as many of these contain milk and sugars, which can actually be more harmful for someone with a difficulty in breaking down lactose, or with bacterial imbalances, which may feed on sugar.
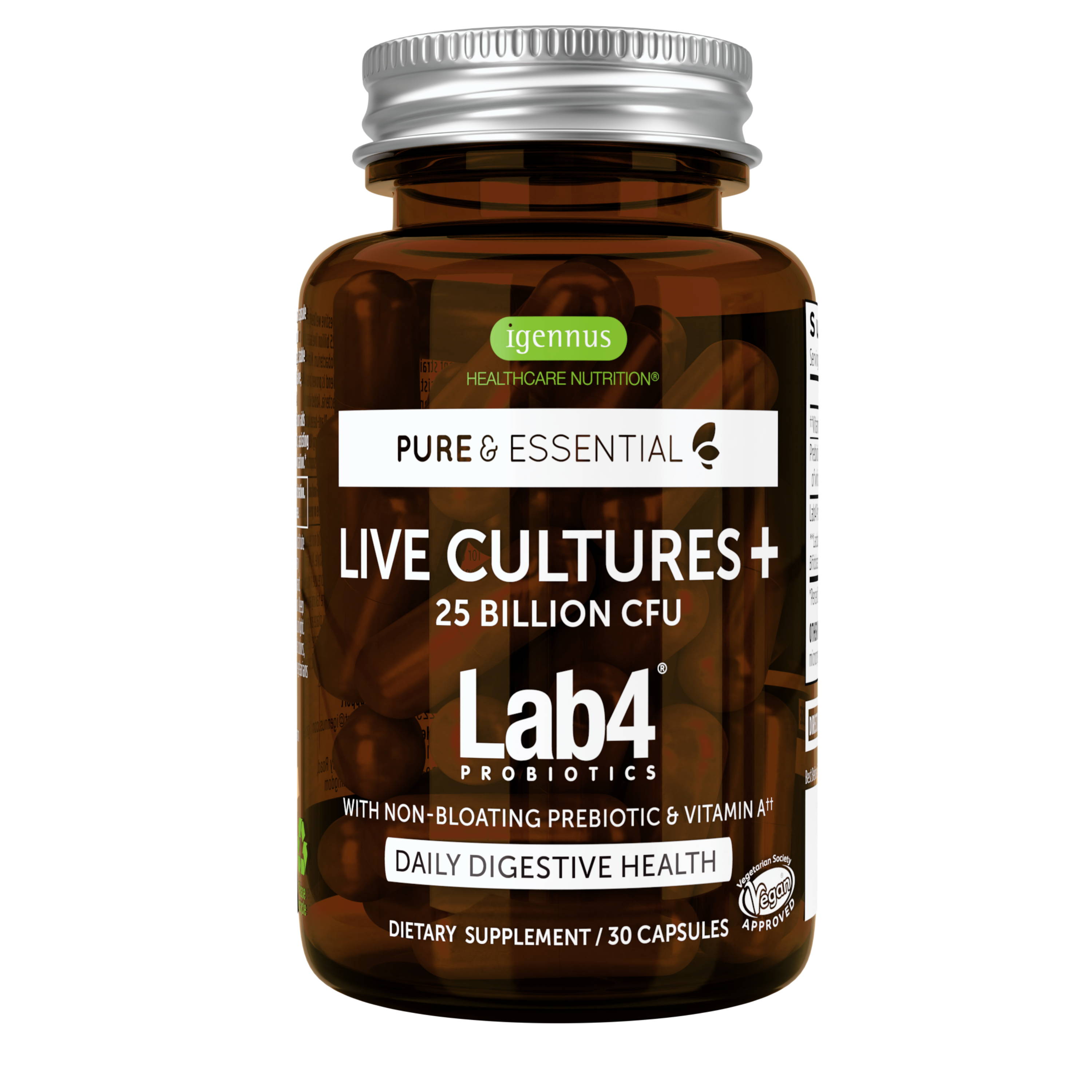
Taking a probiotic for IBS symptoms, including bloating, is the ideal solution with a high strength probiotic capsule containing at least 10 billion probiotic microorganisms, or 25 billion for an intensive dose. Ensuring that probiotic strains are acid-resistant is also key when choosing a probiotic, to increase their chance of surviving stomach acid and colonising in the gut. Live Cultures+ provides a blend of four extensively researched strains of Lab4 probiotics®, including Lactobacillus acidophilus and Bifidobacterium. Bottled at a dose of 50 billion live bacteria, Live Cultures+ Lab4 Probiotics® guarantees 25 billion live bacteria at expiry. We prioritise using fewer strains at higher doses to ensure that a high number of live bacteria reach the intestine walls. Studies have shown that this blend of live bacteria achieved a significant reduction in days with pain and bloating, significantly reduced total symptoms and improved quality of life in diagnosed IBS sufferers. (7)
HEALTHY GUT BACTERIA THRIVE WITH PREBIOTICS

To support colonisation, most prebiotics work by feeding bacteria in the gut, allowing them to multiply. Fructooligosaccharide (FOS) is a prebiotic often found in probiotic supplements and is naturally occurring in foods such as onions, garlic, chicory and artichoke. While FOS is usually effective at improving levels of gut flora, a very common side effect with this prebiotic is excessive gas and bloating.
To reduce bloating side effects, Live Cultures+ Lab4 Probiotics provides Aquamin® - an effective prebiotic derived from algae which acts as a protective carrier for probiotics, transporting more live bacteria to the intestines, instead of feeding bacteria. Aquamin also provides a source of plant-based calcium which helps to neutralise hydrochloric acid within the stomach, protecting live cultures. Additionally, calcium also helps to balance gut flora by creating a favourable pH in the intestines to encourage growth of beneficial bacteria, and supports the production of digestive enzymes.
KEEP YOUR GUT LINING HEALTHY AND CALM
In a healthy digestive tract, the cells lining the intestines are plumped up and closely packed together, carefully controlling the absorption of nutrients from food, keeping the gut calm.
If the gut lining is damaged, however, you may experience painful cramping or sensitivity to foods along with bloating. When mucosal cells covering your intestines become impaired, this is often referred to as ‘leaky gut’ as damaged cells may allow food particles and bacteria to pass through the gut lining. One of the main issues with undigested food particles passing the gut barrier is that it can initiate an immune response, often developing into food intolerances. (3)
There is no one simple cause of a 'leaky gut', however a combination of chronic inflammation, nutritional deficiencies, improper digestion and high intake of commonly aggravating foods such as gluten and alcohol may be to blame. (8, 9) Other possible causes of a permeable gut lining can include parasites and bacterial and yeast infections. An invasion of these pathogenic ‘bad’ bacteria can easily result in inflamed and irritated cells lining the gut and increased level of toxins, which may be released from the pathogens.
You can protect your gut lining by limiting aggravating foods and taking supplements such as digestive enzymes and probiotics to support digestion and balance gut flora. For additional support for gut barrier integrity, consider taking a vitamin A supplement. Vitamin A helps to maintain normal mucous membranes and has a role in the process of cell specialisation, a process that occurs after cell division where newly formed cells develop to function efficiently. Vitamin A is included as beta carotene, a safe and vegan alternative to retinol, in our Live Cultures+ Lab4 Probiotics to support the health of the gut lining.
REFERENCES
(1) Zhu Y, Zheng X, Cong Y, Chu H, Fried M, Dai N, et al. Bloating and distention in irritable bowel syndrome: the role of gas production and visceral sensation after lactose ingestion in a population with lactase deficiency. Am J Gastroenterol 2013 Sep;108(9):1516-25.
(2) Staudacher HM, Whelan K, Irving PM, Lomer MC. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet 2011 Oct;24(5):487-95.
(3) Fedewa A, Rao SS. Dietary fructose intolerance, fructan intolerance and FODMAPs. Curr Gastroenterol Rep 2014 Jan;16(1):370.
(4) Choi YK, Kraft N, Zimmerman B, Jackson M, Rao SS. Fructose intolerance in IBS and utility of fructose-restricted diet. J Clin Gastroenterol 2008 Mar;42(3):233-8.
(5) Karalus M, Clark M, Greaves KA, Thomas W, Vickers Z, Kuyama M, et al. Fermentable fibers do not affect satiety or food intake by women who do not practice restrained eating. J Acad Nutr Diet 2012 Sep;112(9):1356-62.
(6) Ringel-Kulka T, Palsson OS, Maier D, Carroll I, Galanko JA, Leyer G, et al. Probiotic bacteria Lactobacillus acidophilus NCFM and Bifidobacterium lactis Bi-07 versus placebo for the symptoms of bloating in patients with functional bowel disorders: a double-blind study. J Clin Gastroenterol 2011 Jul;45(6):518-25.
(7). Williams EA et al 2008. Clinical trial: a multistrain probiotic preparation significantly reduces symptoms of irritable bowel syndrome in a double-blind placebo-controlled study. Alimentary Pharmacology & Therapeutics, 29: 97-103
(8) Vazquez-Roque MI, Camilleri M, Smyrk T, Murray JA, Marietta E, O'Neill J, et al. A controlled trial of gluten-free diet in patients with irritable bowel syndrome-diarrhea: effects on bowel frequency and intestinal function. Gastroenterology 2013 May;144(5):903-11.
(9) Elamin E, Jonkers D, Juuti-Uusitalo K, van IS, Troost F, Duimel H, et al. Effects of ethanol and acetaldehyde on tight junction integrity: in vitro study in a three dimensional intestinal epithelial cell culture model. PLoS One 2012;7(4):e35008.