Thyroid problems are usually easy to identify for their several negative health effects that impact not only metabolism and weight management, but also digestion, skin health and many more areas of our physiology. Difficulty in losing weight is a common complaint in clinic, amongst other health issues which may arise due to dysregulated thyroid function. Subclinical thyroid dysfunction, particularly hypothyroidism, is rarely identified and diagnosed by the GP. Understanding the functions of the thyroid gland in detail, and how to perform tests sensitive enough to identify hyper- or hypofunction, is important in order to better support and optimise your client’s thyroid function through nutrition and lifestyle interventions.
Function of the thyroid gland
Positioned in the neck, just below the thyroid cartilage, the thyroid gland surrounds the trachea. As an endocrine gland, the thyroid gland secretes hormones directly into the blood, determining the metabolism of every cell in the body. T4, T3 and calcitonin are the three hormones released from the thyroid gland. T4 (thyroxine) and T3 (triiodothyronine) are important for growth and development, whilst calcitonin supports calcium and phosphate homeostasis in the body, by increasing calcium delivery to and deposition in the bones, whilst preventing its reabsorption and is therefore essential for healthy bone development.
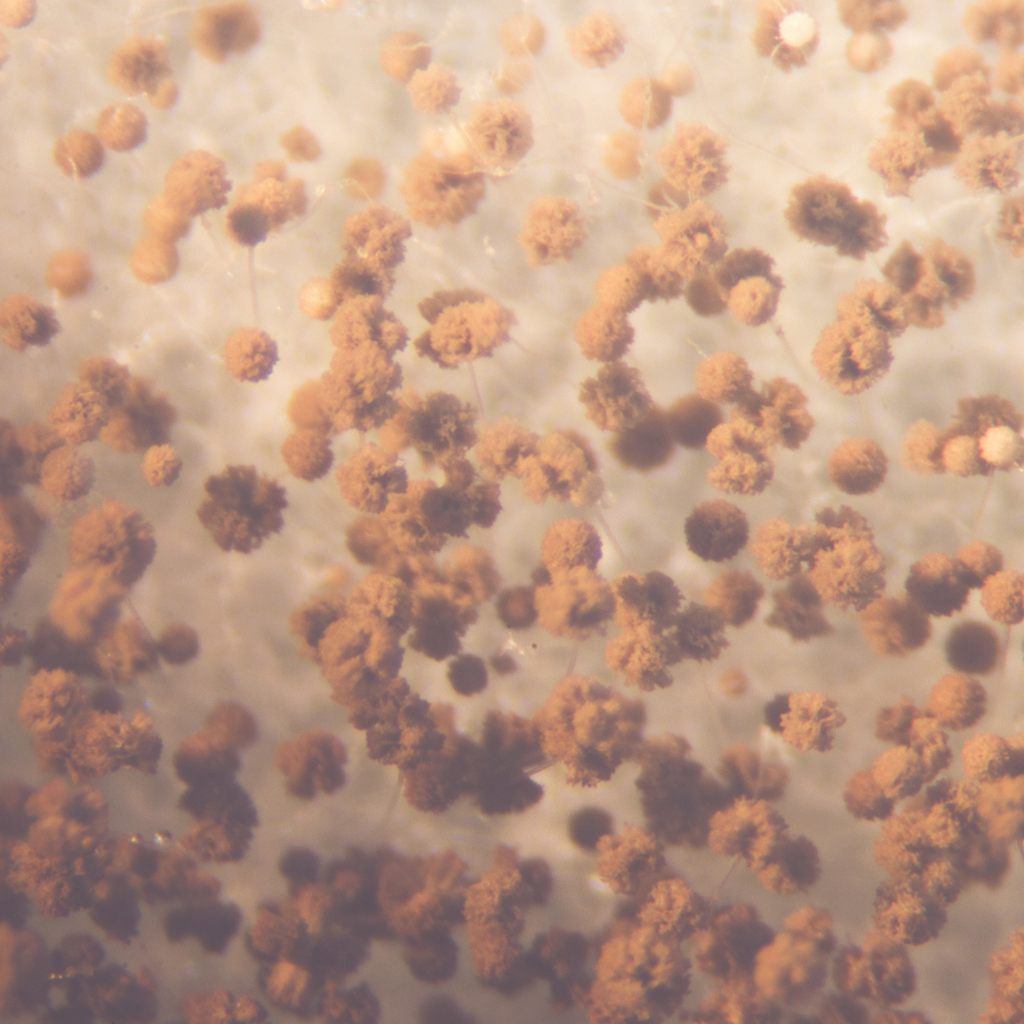
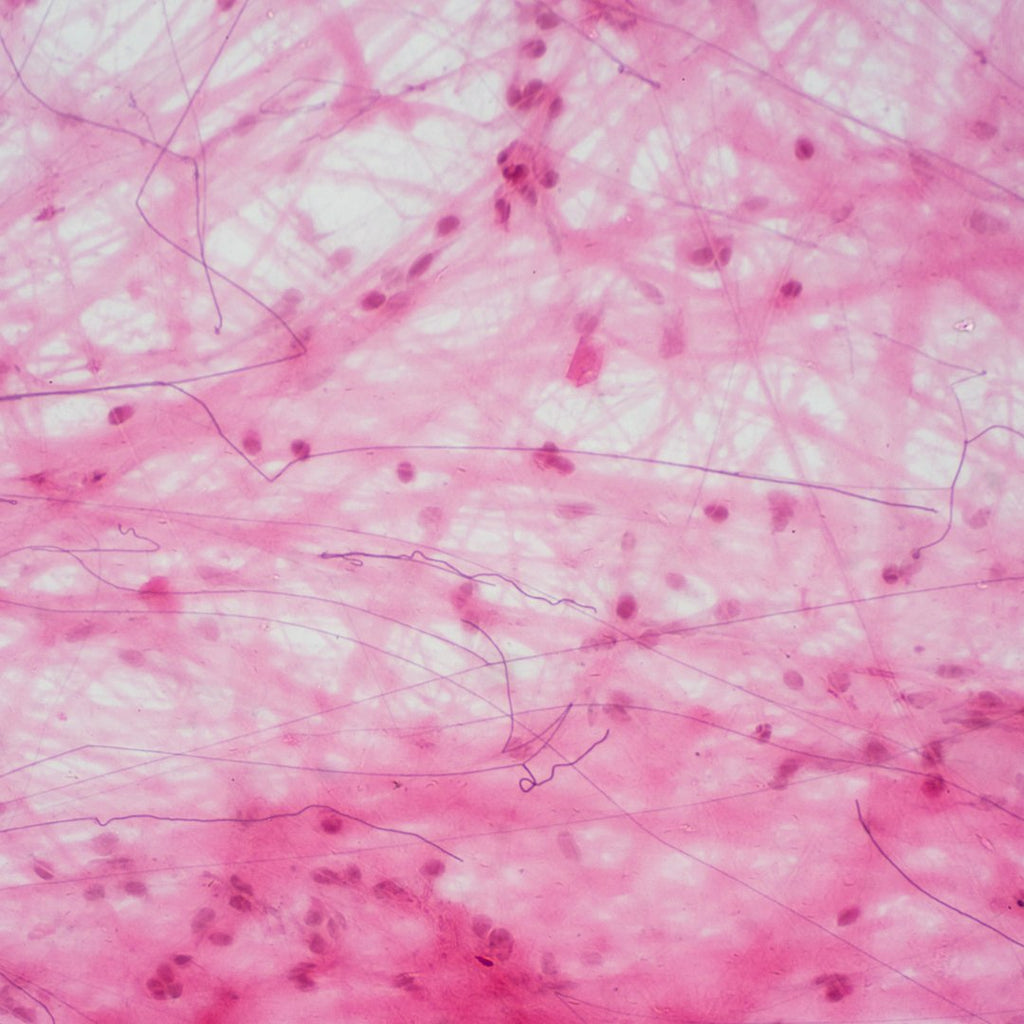
The surface of the thyroid gland is covered in follicles which are constantly absorbing iodine, and is surrounded by a single layer of epithelial cells. Two different types of cells secrete hormones from the thyroid gland: follicular cells secrete T4 and T3, and parafollicular cells secrete calcitonin.
The thyroid gland is sometimes confused with the parathyroid glands, four very small glands positioned on the back of the thyroid gland, which perform a completely different role in the body from that of the thyroid. The parathyroid glands release parathyroid hormone (PTH) which causes osteoclasts to break down bone to release calcium and therefore increase levels of calcium in the blood, the opposite effect to that of calcitonin.
The production of the hormones T4, T3 and calcitonin actually begins at the hypothalamus which secretes TRH, resulting in the pituitary gland secreting thyroid-stimulating hormone (TSH) which finally stimulates the thyroid gland to produce T4, T3 and calcitonin. To prevent constant stimulation of the thyroid gland, the body has a negative feedback loop: when T4 levels are high, a message is fed back to the pituitary gland to reduce production of TSH, thus slightly reducing thyroid hormone production. Other states, such as exposure to cold, would have an opposite effect by increasing production of TRH from the hypothalamus, thereby increasing TSH production, stimulating the thyroid to increase thermogenesis to heat up the body. High levels of iodine, steroids and sex hormones such as high oestrogen can have a negative effect on the thyroid gland by reducing TSH production.
The thyroid produces both T4 and T3 in the body, with T4 being produced at a much higher rate, up to 20:1 in some cases. T3 is the most biologically active of the two, however, and is therefore more effective at regulating growth and metabolism. Conversion in the body from T4 to T3 occurs not only in the thyroid gland but also in other glands such as the liver, kidney and spleen. If the conversion is not optimal, whether due to mineral deficiency, poor liver function or adrenal issues, this may result in high, or normal T4, but low T3. This could result in low TSH if both T4 and T3 are quite low, but if T4 is normal and only T3 is low, TSH levels may be normal. This helps to explain why measuring TSH levels is not always the best indicator for metabolism and other functions of T3, as this could be low because of conversion problems. Hormones T4 and T3 also need to be in their free form - cleaved from their protein carriers - in order to be used by cells.
Thyroid dysfunction
Thyroid dysfunction can exist for many different reasons: most commonly presented to nutritional therapists may be hypothyroidism, whereby the thyroid gland is underactive; hyperthyroidism, in which the thyroid gland is overactive, may also present. Other thyroid conditions include thyroiditis, inflammatory conditions of the thyroid gland, and thyroid nodules or cancer.
Hypothyroidism (underactive thyroid)
An underactive thyroid results in the low production of T4 and T3 hormone, which usually (not always) corresponds with a high production of TSH released from the pituitary gland to try to compensate for these low levels by further stimulating the thyroid gland. An underactive thyroid may be a result of nutritional deficiencies of iodine or tyrosine, due to a lack of the building blocks being available to synthesise thyroid hormones. Other possible causes include thyroid abnormalities from birth, autoimmune conditions such as Hashimoto’s, and surgical removal of the thyroid gland, usually following a cancer diagnosis.
Symptoms of an underactive thyroid include weight gain, or difficulty losing weight due to a decreased metabolism, sensitivity to cold due to lower levels of thermogenesis in the body, and a swollen neck (goitre). With the slowing down of systems in the body, other symptoms such as brittle hair, brittle nails and dry skin can also result. In addition to these symptoms, hypothyroiditis can also have an impact on several other systems in the body, resulting in sluggish digestion, constipation (in most cases) and reduced fertility.
Hyperthyroidism (overactive thyroid)
An overactive thyroid results from an over-production of hormones T4 and T3. Causes of such problems are usually a result of an autoimmune disease such as Grave’s disease, in which antibodies attack the tissues of the thyroid gland. This can also result in the breakdown of tissues behind the eyes, which can give the appearance of bulging eyes. Grave’s disease is considered to have a possible genetic predisposition. Other conditions, such as Plummer’s disease and thyroiditis, can also lead to hyperthyroidism. An overactive thyroid is essentially overstimulated, as the negative feedback loop usually in place to modulated hormone production is lacking. An overworked thyroid can result in an enlarged thyroid gland, causing swelling in the neck, as well as other symptoms including weight loss, or difficulty putting on weight, an elevated heart rate and reduced fertility. An overactive thyroid can also increase cells’ sensitivity to adrenaline, which can increase feelings of stress and anxiety. With a speeded metabolism, processes such as skin growth can also increase, causing excess skin tissue growth, commonly resulting in the appearance of thick skin on the lower legs, giving an appearance similar to psoriasis. Digestion is also affected, with transit time reduced, commonly leading to diarrhoea.
Thyroiditis
Inflammation of the thyroid gland is usually a result of a condition such as Hashimoto’s, de Quervain’s or postpartum thyroiditis, although fluctuating levels of thyroid hormones can also cause additional inflammation. An individual with fluctuations between hypo- and hyper-thyroiditis may, therefore, have an inflamed thyroid gland causing additional strain.
For anyone with suspected inflammation of the thyroid gland, it may be worth addressing their diet to keep inflammation at a healthy level. Managing the omega-6 AA to omega-3 EPA ratio is the most effective method for achieving this, with an ideal ratio of 3:1. If inflammation is high and consumption of inflammatory fats such as from grain-fed meats, grains and vegetable oils is high with low fish intake, this may indicate chronic inflammation.
Nodules and cancer
If for any reason you suspect that something is severely wrong with the thyroid - for example, if your client complains about abnormal lumps on their neck - the possibility of nodules or cancerous growths must be considered. If in any doubt, refer your client to their GP for a check-up. It is worth noting that nodules and cancerous growths may occur with or without pain.
GPs may carry out a physical examination over the outside of the neck, feeling for abnormal growths or swelling. The thyroid gland cannot usually be felt unless there are problems resulting in excess growth which is often picked up by a GP. Blood tests may also be offered to test for T4 and levels of thyroglobulin, the protein produced in the thyroid gland. If levels are high, this may suggest excess tissue growth of the thyroid gland as tumours can increase the production of thyroglobulin.
If something shows up on initial tests, a neck ultrasound may be administered to view abnormalities, and preceding this, possibly a CT scan, MRI scan or PET scan.
Diagnostic tests
When considering tests, it may be worth starting off with a basal temperature test, which can be carried out by your client at home. A simple measure of body temperature using a thermometer under the arm upon waking is usually a good indicator of thyroid function if you are aiming to determine hypo- or hyperthyroidism. Someone with an underactive thyroid gland is likely to have a fairly low body temperature upon waking, i.e. below 36 deg C. Please note that body temperature thermometers often present a temperature approximately a degree lower than internal body temperature, therefore a reading of 36.5 deg C is considered normal.
When considering blood tests and urine tests, it may be worth measuring T4, T3, free T4, free T3, and TSH in order to understand hormone production by the thyroid gland, as well as to understand the conversion of T4 to T3 in the body. If results present a healthy or high level of T4, but a low level of T3, consider conversion issues. High TSH levels also usually indicate hypothyroidism as a mechanism to try to stimulate the thyroid gland. You may also wish to consider testing reverse T3, which is a metabolite of T4, although an inactive form. If someone has healthy T4, but is converting this to the inactive form of T3, this could present as an underactive thyroid. Antibodies such as anti-TG and anti-TPO can also be tested for, to identify conditions such as Grave’s disease and Hashimoto’s thyroiditis. (1)
Comparing the efficacy of blood tests vs urine tests, urine tests are much more sensitive, measuring levels of free T4 and T3 over a 24-hour period. Although blood tests are the most commonly used to diagnose thyroid conditions, urine tests may be more suitable when considering subclinical hypothyroidism. Reference ranges used by GPs are also fairly wide, as they are intended to identify serious thyroid conditions rather than a sub-functioning thyroid. If a client comes to you explaining that their GP has tested their thyroid function and everything is totally normal, it may be worth considering that they may have had their blood levels tested for T4 and thyroglobulin, which would not pick up mild hypothyroidism.
Nutritional support
Tyrosine and iodine
The body requires a supply of tyrosine and iodine to synthesise T4 and T3 hormones; for optimum thyroid function, therefore, healthy levels should be included in the diet.
Tyrosine is an amino acid found in foods such as eggs, cheese and turkey. Tyrosine can also be synthesised from the amino acid phenylalanine (found in foods such as chicken, fish, cheese and beans). Ensuring adequate protein-rich foods are in the diet will improve tyrosine levels. Tyrosine can be supplemented for those who really need it - for example, if someone’s dietary intake of tyrosine is very low, or if they have digestive issues. 500-1000mg before each main meal is sufficient. It must be noted that supplementing high-dose tyrosine can have negative effects for some individuals so should be carried out with caution: bipolar symptoms may be exacerbated, and it is also not recommended for anyone with significantly high blood pressure. If someone is already taking thyroid medication, they would also not be recommended to take tyrosine, to avoid overstimulation of the thyroid gland. Tyrosine supplementation at high dose can also result in digestive discomfort and migraine in some individuals.
Iodine is a trace element found in foods such as seaweed, fish, seafood and eggs. Levels may therefore be quite low if someone is following a vegetarian or vegan diet. Iodine is absorbed into the thyroid gland through follicles, and then stored in thyroglobulin. When considering dietary iodine intake, consider that too little or too much may cause issues. Supplementing with iodine in high doses is, therefore, not always suitable. Ensuring good levels of iodine are consumed in the diet should be top of your list, however. (2) Deficiency of iodine may present as stunted growth and brain developmental delays. Note that some vegetables contain goitrogens, which can actually block absorption of iodine. (See Foods to avoid, below)
Micronutrients
Ensure healthy intake of micronutrients which are particularly required for thyroid health, including zinc (3), iron and copper sourced from foods such as grass-fed meats, nuts and seeds and perhaps supplements in those who may find it difficult to obtain these directly from their diet.
An antioxidant-rich diet should, of course, be included in a nutritional programme to support thyroid health in order to reduce oxidative damage, reducing thyroid tissue cell damage, with particular attention to selenium (2;6) and vitamin E. (7)
Inflammation
Inflammation levels must be considered for anyone with thyroid problems to protect against damage and to reduce the additional burden on the thyroid gland. Fish is one of the healthiest foods to consume, both for its anti-inflammatory omega-3 fatty acids (4) and for its content of iodine and tyrosine.
Omega-3 EPA is particularly effective at reducing inflammation, as well as increasing production of T4 (5) and improving sensitivity to thyroid hormones. For those with low or no consumption of fish or for those with possible inflammation or poor dietary choices, consider a high strength omega-3 EPA supplement. The dose of EPA should, ideally, be around 1000mg EPA to reach the therapeutic anti-inflammatory effects, and EPA on its own without DHA is most effective in terms of reducing inflammation. Pharmepa RESTORE, 2 a day with food would be suitable for at least 3 months, providing a 90% concentration of EPA in small capsules, and derived from wild anchovies, a sustainable source certified free from methyl mercury, PCBs and dioxins.
Foods to avoid
A few foods to possibly avoid for someone with thyroid problems: firstly, anything artificial, such as aspartame; although there are limited studies carried out in this area, there is certainly a lot of anecdotal evidence to suggest that cutting out artificial ingredients can help to give the thyroid a break and speed up recovery. Oestrogenic chemicals found in plastics and soy may also be worth cutting out; with their effects on the body similar to oestrogen (8), TSH production from the pituitary gland can be reduced, causing reduced thyroid activity.
Goitrogen-containing foods such as spinach, Brussels sprouts, broccoli and strawberries should be cooked to avoid their effects on reducing iodine uptake. There is no need for anyone to totally cut out these healthy foods, although fully steaming them would be appropriate. Gluten may also have a negative effect on the thyroid gland, mostly by increasing inflammation in the body, but also by intolerances cross-reacting, therefore exacerbating autoimmune diseases.
Lifestyle factors
Lastly, always be sure to recommend a lifestyle which supports thyroid health. It is likely that if you have a client with hypothyroidism, they will be watching their calorie intake and doing extreme exercise to lose weight; more often than not, though, this leads to nutritional deficiencies and a struggling thyroid gland. Such exercise can be too intense, therefore consider more relaxing forms of exercise such as yoga and gentle swimming for a phase of approximately three months. Explain to your client this is important and necessary in the early phase of optimising thyroid health. Stress release, relaxation, rest and adequate sleep are all paramount in ensuring proper functioning of the thyroid gland.
References
- Naiyer AJ, Shah J, Hernandez L, Kim SY, Ciaccio EJ, Cheng J, et al. Tissue transglutaminase antibodies in individuals with celiac disease bind to thyroid follicles and extracellular matrix and may contribute to thyroid dysfunction. Thyroid 2008 Nov;18(11):1171-8.
- Triggiani V, Tafaro E, Giagulli VA, Sabba C, Resta F, Licchelli B, et al. Role of iodine, selenium and other micronutrients in thyroid function and disorders. Endocr Metab Immune Disord Drug Targets 2009 Sep;9(3):277-94.
- Kuriyama C, Mori K, Nakagawa Y, Hoshikawa S, Ozaki H, Ito S, et al. Erythrocyte zinc concentration as an indicator to distinguish painless thyroiditis-associated transient hypothyroidism from permanent hypothyroidism. Endocr J 2011;58(1):59-63.
- Wall R, Ross RP, Fitzgerald GF, Stanton C. Fatty acids from fish: the anti-inflammatory potential of long-chain omega-3 fatty acids. Nutr Rev 2010 May;68(5):280-9.
- Taraghijou P, Safaeiyan A, Mobasseri M, Ostadrahimi A. The effect of n-3 long chain fatty acids supplementation on plasma peroxisome proliferator activated receptor gamma and thyroid hormones in obesity. J Res Med Sci 2012 Oct;17(10):942-6.
- Stazi AV, Trinti B. Selenium status and over-expression of interleukin-15 in celiac disease and autoimmune thyroid diseases. Ann Ist Super Sanita 2010;46(4):389-99.
- Venditti P, Di SL, Di MS. Vitamin E management of oxidative damage-linked dysfunctions of hyperthyroid tissues. Cell Mol Life Sci 2013 Sep;70(17):3125-44.
- Sathyapalan T, Manuchehri AM, Thatcher NJ, Rigby AS, Chapman T, Kilpatrick ES, et al. The effect of soy phytoestrogen supplementation on thyroid status and cardiovascular risk markers in patients with subclinical hypothyroidism: a randomized, double-blind, crossover study. J Clin Endocrinol Metab 2011 May;96(5):1442-9.