The benefits of omega-3
Although omega-3 was a hot topic throughout 2018, recent studies are showing us that there is a clear difference between how much omega-3 we think we consume and how much we actually consume. Consequently, the majority of people will have suboptimal levels, putting them at risk for developing poor health. Clearly there is an urgent need to increase public awareness, not just of how essential omega-3s are to our health, but more so because of the consequences that can arise when levels decrease. In this article, we discuss the benefits of testing and the common issues associated with raising and maintaining a healthy omega-3 status and how to overcome them.
As omega-3s play such a fundamental role in most body processes, we should aim to consume EPA & DHA daily in order to satisfy high requirements for it, either by diet, supplements or both; however, without guidance on the ideal ‘target’ level we should aim for, and with an individual’s omega-3 needs specific to them, it can be challenging to know just how much should be consumed daily. Measuring the amount of omega-3 that makes up the framework of our cells and tissues and expressing this as a simple number or ‘index’ provides us with a useful biomarker to estimate omega-3 intake. It is not uncommon for healthcare providers to use numbers to create a picture of a person’s general health status and then provide improvement guidance. For example, it’s common knowledge that we should keep our cholesterol below 5 or that blood pressure should not exceed 120 over 80. The Omega-3 Index (derived by calculating the amount of EPA & DHA in our cell membranes and expressed as a %) takes the use of health biomarkers to a higher level by providing us with a comprehensive overview of our total health. Achieving an Omega-3 Index of 8-10% has been scientifically validated as optimal, with studies showing a direct correlation between the Omega-3 Index and the risk of developing cardiovascular disease, dementia, inflammatory conditions and even type II diabetes - the higher the index, the lower the risk. As a ‘health’ biomarker, the Omega-3 Index is incredibly robust and easily manipulated by diet and/or supplements, yet communication of its value, certainly to the general public, is lacking. By encouraging consumers to become self-aware regarding their omega-3 levels, an ‘at-risk’ health status can motivate them to tackle the problem, because once their Omega-3 Index is known, the appropriate action can be taken to achieve the target 8-10%. While raising an Omega-3 Index should be relatively straightforward, there are a number of potential barriers that can affect how successful an intervention is.
Fishy facts – why oily fish is an unreliable source of omega-3
When considering foods that supply omega-3 fatty acids, we probably think first of fish. Looking at the evidence provided by epidemiological studies, it is clear that those individuals who eat fish on a regular basis typically experience better health and greater longevity than those individuals who do not eat fish (they also have higher omega-3 levels); however, while it is tempting to suggest that these benefits are directly related to the omega-3 content, it's acknowledged that people who eat fish are, on the whole, likely to be more health‐conscious than those who do not. It’s also worth highlighting that, in addition to being a potentially rich source of EPA & DHA, fish is also known to be a good source of other health-promoting nutrients including calcium, iodine, selenium, zinc and protein. A healthy fish-based meal may also displace a variety of other potentially less healthy foods. As such, the benefits that can be gained from eating oily fish weekly cannot be overstated, yet most people in the UK consume considerably less than the recommended one portion of oily fish per week. In addition, we cannot categorically state that the benefits from eating fish are derived solely from the omega-3 content, not only because the level of omega-3 found in oily fish is declining, but also because eating fish is highly confounded by numerous factors including dietary quality, socioeconomic status and other markers of ‘healthy’ lifestyles.
While public consensus places fish as the ‘healthier’ choice, much of that consumed in the UK is now intensively farmed, prompting considerable doubt over its potential nutritional quality. In addition, the levels of EPA and DHA in the flesh of farmed fish have fallen significantly in recent years due to the increased use of cheap rapeseed oil in place of the more expensive fish oil used in aquafeed. For example, in 2006, an average 140g portion of Scottish Atlantic salmon would have delivered 3.84g EPA & DHA (~0.54g per day if eaten once weekly) which had dropped to 1.9g per 140 g by 2015 (~0.27g per day). This means that an individual now needs to consume oily fish twice per week to achieve the government recommended daily intake of 450mg EPA & DHA (Sprague et al. 2016). Given that the government guidelines on oily fish consumption as a source of omega-3 remains at a single 140g portion weekly, it is not surprising that many people overestimate how much omega-3 they consume. In fact, the average EPA and DHA intake in the UK is believed to be less than 250mg/day (Micha et al. 2014) which reflects the sub-optimal omega-3 status of the population as a whole (Stark et al. 2016). It’s estimated that, on average, a person would need to maintain an intake of 1-2g EPA and DHA daily to raise levels from sub-optimal to optimal and to preserve healthy levels of omega-3, the equivalent of eating 140g oily fish each day (Jackson et al. 2019).
The Omega-3 Index as a biomarker of intake
Not only is fish rapidly becoming less reliable as a source of omega-3, but the numerous health benefits provided by fish consumption may be compromised by the presence of metals and other pollutants which can have harmful effects on the human body if consumed in toxic quantities. With low EPA and DHA status associated with an increased risk of chronic disease, the most effective way to ensure a guaranteed regular intake of a known amount of EPA & DHA with the aim of raising omega-3 status to optimum is by taking a fish oil supplement. Unfortunately, the fish oil industry is a booming market saturated with products that differ significantly in quality, and with manufacturers adopting quite manipulative and misleading marketing techniques, it can be very challenging for both consumers and practitioners to be confident that the fish oil they choose will be effective at raising omega-3 levels. Unless a product addresses potential barriers such as strength, dose & bioavailability, it is unlikely that it will be able to achieve omega-3 levels required to have a significant impact on reducing risk markers (Laidlaw et al. 2014). So, while supplementing with fish oil may be the most effective way of delivering omega-3, merely taking fish oil does not guarantee high levels of EPA and DHA. Given that between 1-2 grams may be needed to achieve an omega-3 index of ≥8%, with as much as 4 grams required for clinical effect, the ‘ideal’ supplement should be able to deliver a therapeutic dose as highly-bioavailable, highly-concentrated EPA/DHA.
*Flock et al. 2013
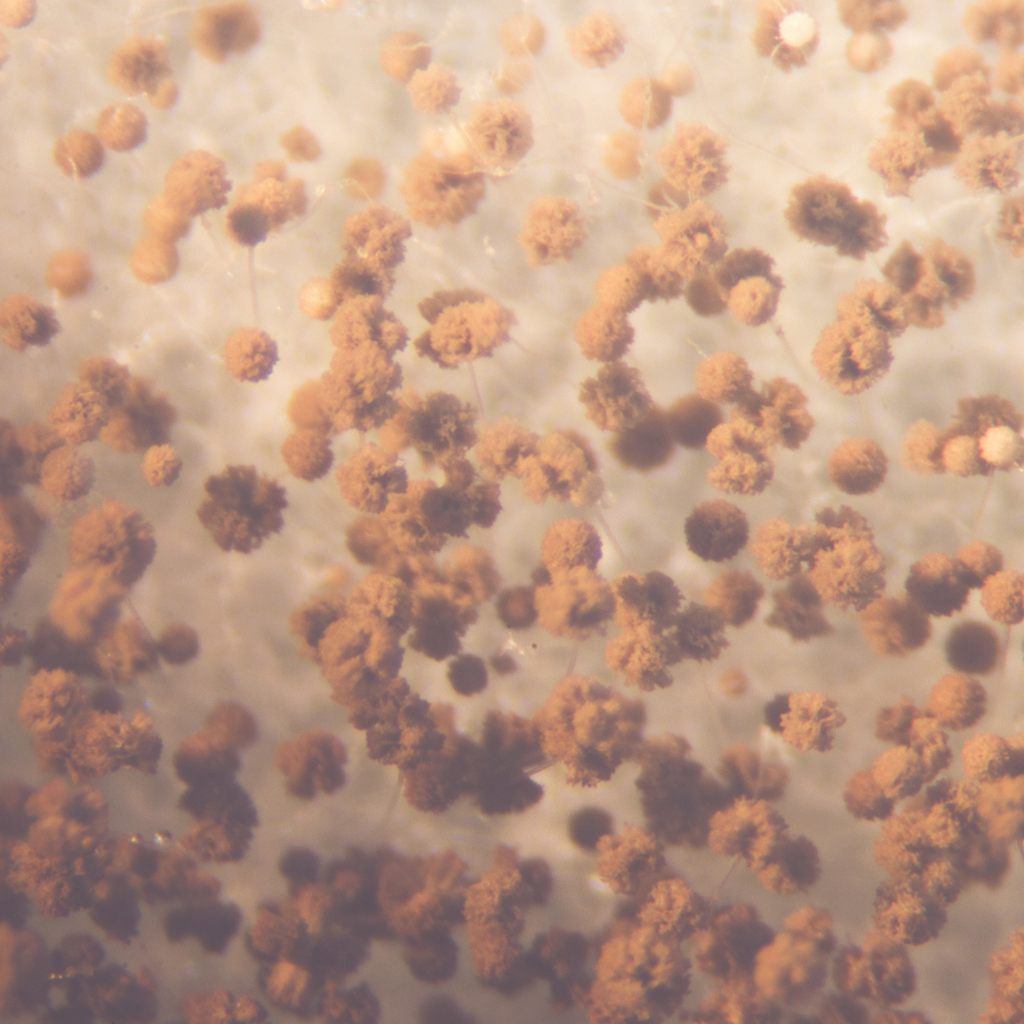
To appreciate the potential impact that omega-3 fatty acids may have on the body in terms of disease risk reduction, we need to look at how effective a fish oil product is at raising body levels of these important fats. With an average 80—120-day life span, red blood cells (RBCs) provide a reliable and robust biomarker of long-term dietary intake of omega-3, with RBC membrane levels correlating highly with body tissue levels in the gut, heart, liver and kidney. The Omega-3 Index is a well-established, validated biomarker of omega-3 levels that reflect dietary intake and correlates strongly with cardiovascular health. The Omega-3 Index is now widely accepted within the scientific community as a biomarker of cardiovascular disease (CVD - the umbrella term for all types of diseases that affect the heart or blood vessels) risk that has been shown to be significantly more robust as a biomarker of risk than C-reactive protein, cholesterol, triglycerides or homocysteine (Harris 2007). As the use of the Omega-3 Index as a health biomarker is not limited to CVD, it stands to reason that there are benefits to gain from its broader application and communicating this to the broader public with the aim of reducing disease burden and the associated health costs.
Measuring the Omega-3 Index is more valuable than measuring cholesterol
It has long been considered that raised cholesterol is a key cause of the fatty build-up in arteries (atherosclerosis) that causes coronary heart disease (CHD). While monitoring cholesterol levels has for decades been seen as the most appropriate indicator of a person's risk of having a heart attack, recent evidence suggests that the Omega-3 Index may be significantly more reliable. The relationship between the Omega-3 Index and the risk for CHD-related death (heart attack associated with atherosclerosis) was evaluated in 2004 by Harris & Von Schacky, who reported (from published primary and secondary prevention studies) a direct association between the Omega-3 Index and the risk of death from a heart attack. Individuals with an Omega-3 Index of ≥8% benefited from the greatest cardio-protection, whereas individuals with an index ≤4% were at the highest risk of dying (Harris &Von Schacky 2004). These cut-offs have been replicated on numerous occasions and in his 2017 paper, Harris, using published data from 10 cohorts (n = 27,505) measuring RBC EPA & DHA levels, was able to report their estimated mean Omega-3 Index equivalents to determine the risk of death. The overall mean Omega-3 Index for the ten studies was 6.1%, the median value for the lowest quintile (Q1) was 4.2%, and the median value for the highest quintile (Q5) was 8.3%. Using linear analysis, it was estimated that increasing the Omega-3 Index from 6.1% to 8.3% could reduce the risk of dying from a fatal heart attack by around 15% and that by raising it from 4.2% to 8.3% could reduce this risk by a staggering 30% (Harris et al. 2017).
The robustness of the Omega-3 Index in comparison to cholesterol levels has most recently been reported in the Framingham Offspring study (children of the original 1948 Framingham study participants). The study repeatedly measured the omega-3 status of 2500 people (recruited at age 66) over a period of 7 years. At the end of the study, those individuals in the highest (>6.8%) compared to those in the lowest Omega-3 Index quintiles (<4.2%) had a 34% lower risk of death from any cause and 39% lower risk of CVD. A high Omega-3 Index was associated with a lower risk for total CVD events, total strokes and was found to be a more accurate predictor of CVD than serum cholesterol, which has been for many years viewed as a ‘gold standard’ risk factor for predicting heart disease. (Harris et al. 2018)
While the majority of individuals have a general understanding of the link between high cholesterol and cardiovascular disease, the safety of statins as cholesterol-lowering drugs is often raised as a concern due to their potential side effects, and the public often sees the restriction of certain foods, required to help reduce cholesterol, as challenging.
In contrast to cholesterol reduction, raising omega-3 levels to reduce CVD risk is not only significantly more straightforward but offers benefits that go well beyond cardiovascular health alone. With the average omega-3 index in the UK less than 4%, it stands to reason that benefits should be gained from raising the Omega-3 Index to 8% or higher and, because altering the Omega-3 Index is simple, safe and relatively inexpensive, it may be especially useful for those individuals known to be at a higher risk of chronic disease including CVD. In addition, cholesterol-lowering is a known ‘side effect’ (or, more accurately, ‘side benefit’) of omega-3s. Several trials (ANCHOR, REDUCE-IT, MARINE & JELIS) have demonstrated significant triglyceride- and cholesterol-lowering benefits of pure EPA that then translates to reduced cardiovascular ‘events’.
Issues with estimating omega-3 intake
It is important to consider the amount of EPA & DHA an individual might need to consume to move them from a level of high risk (<4%) into a cardio-protective range (>8%). In a 2017 survey, US physicians were questioned about their omega-3 intake; while 51% (173/340) reported that they felt they consumed adequate omega-3 to push them into the desirable range, only 5% (17/320) had an Index ≥8%. The average Omega-3 Index was 5.2%, and the average AA to EPA ratio (as a biomarker of the body’s inflammatory potential) was 13, with only 3 (0.8%) having a ratio within the desirable range (<3). This finding suggests that many US physicians are unaware of their omega-3 status and how it relates to their daily dietary habits, something possibly true of UK GPs/doctors. Interestingly, 27% fell into the category of consuming fatty fish ≥ 2x/week and omega-3 supplements >5x/week (Matusheski et al. 2017). Similarly, in a cross-sectional survey of adults living in Germany and the USA, asked about their knowledge of omega-3 and intake of omega-3 foods (as both fish and supplements), it was common to overestimate their intake as ‘sufficient.' When tested, the average Omega-3 Index values in the USA and Germany were 4.3% and 5.5%, respectively, with 10% of Germans and 40% of Americans with Omega-3 Index < 4%, putting them in the ‘high risk for CVD’ category (Thuppal et al. 2017). Given that omega-3 supplements vary in their omega-3 content, and oily fish is lower now in EPA&DHA than previously, it is easy to see how people can overestimate both their omega-3 intake and their omega-3 status, highlighting the need to educate people about the amount of omega-3 in the food/supplements they use and the benefits of omega-3 testing.
Omega-3 reduces markers of inflammation
A long-standing association exists between elevated triglyceride levels, inflammation and CVD. High levels of inflammatory markers provide predictive measures of both CVD risk and progression, with several studies showing an inverse association between the Omega-3 Index and major biomarkers of CVD-related inflammation including CRP, IL 6 and TNF-α (Fontes et al. 2015). The potential for omega-3 supplements to reduce inflammation was reported in a 2014 meta-analysis of 68 trials that demonstrated an overall significant reduction in CRP and IL-6 and marginally significant reductions in TNF-α after omega-3 supplementation (Li et al. 2014). High triglycerides lead to low-grade inflammation, increased oxidative stress, foam cell formation and formation of atherosclerotic plaques. High levels of triglycerides also activate cholesterol ester transfer protein (CETP) which is important in cholesterol and lipoprotein exchange and results in the reduction of HDL levels. As HDL plays a role in reverse cholesterol transport by removing cholesterol from the tissues and returning it to the liver, low levels of HDL may be a more powerful predictor of heart disease than high levels of LDL. It is accepted that daily doses of 2-4g omega-3 are required to reduce triglycerides (von Shacky 2006). Taking into consideration age, sex and body weight, it is estimated that an individual weighing ~75 kg with a baseline Omega-3 Index of around 4% would require ~1-2g/day of EPA & DHA to raise their omega-3 status to >8% (Katan et al. 1997; Browning et al. 2012; Flock et al. 2013). So while studies do support the use of high dose fish oils, the majority of fish oils available to consumers simply do not supply adequate omega-3 per dose. In 2014 Laidlaw and colleagues studied the efficacy of manufacturers' recommended doses of omega-3 fatty acids from different sources in facilitating cardiovascular disease risk reduction. The average weight of participants was 77kg, and the average baseline Omega-3 Index was 4.18% (high CVD risk). Based on Flock's estimation, the dose required to achieve an omega-3 index of 8% would be in the region of 1.25g. The manufacturer's daily dose of the concentrated rTG oil was 1.1g, the standard fish oil 400mg, and the krill oil 240mg.
In contrast to concentrated rTG fish oil, both krill oil and fish oil were (as expected) unsuccessful in raising the Omega-3 Index (4.93% & 4.76%). The concentrated oil (1g rTG EPA & DHA) raised the Omega-3 Index from 4.17% to 6.82% after 28 days of supplementation. While 1.1g rTG omega-3 fell short of achieving the optimal Omega-3 Index of 8% for reducing CVD risk after 28 days, these results do support those previous studies, demonstrating that significantly higher doses are required to achieve an ideal target range of between 8-10%. Given that in 2016, 62% of adults in England were classified as overweight or obese, it can be estimated that for the majority of individuals taking a standard fish oil supplement based on the manufacturer’s dosing guidance, they are likely to be under-consuming EPA & DHA, thus leaving them considerably short of achieving optimal omega-3 levels. When considering supplementation, the preferential uptake of EPA and DHA by specific phospholipids is highly significant as this influences the amount and the ratio of EPA and DHA required. The majority of EPA is incorporated into phosphatidylcholine (PC) located in the outer membrane of the cell's bilayer. As such, EPA can have a potentially high turnover rate because it is exposed to an environment that allows it to be removed on demand (for eicosanoid production). In contrast, because DHA is preferentially incorporated into phosphatidylethanolamine (PE) and located mainly on the inner membrane of the cell, the majority of DHA stores are protected from the actions of the phospholipase enzymes required to remove fatty acids from cell membranes, meaning that its levels are retained, and its turnover rate is consequentially much slower than that of EPA. As such, supplementing with a product containing a high DHA to EPA ratio when DHA stores are saturated (but EPA levels are low) would be less effective than a supplement containing a high EPA to DHA ratio. The only guaranteed way to ensure healthy levels of EPA and DHA are achieved is by testing baseline omega-3 levels, and then personalising dosing that is not only based on body weight but that also takes into account the appropriate ratio of EPA to DHA required on a case-by-case basis.
The AA to EPA ratio
Omega-6 fatty acids, like omega-3s, are components of cell membranes and are precursors to substances involved in the regulation of cardiovascular health and a healthy inflammatory response. The two families are competitive in nature, with omega-6 considered as predominantly pro-inflammatory and omega-3 anti-inflammatory. While intake of omega-3 is generally low nowadays, our intake of omega-6 has become generally high, which can, over time, lead to a number of health issues. Increased consumption of processed seed and vegetable oils and consumption of intensively farmed animal (and fish) products, coupled with low intake of omega-3 has distorted the delicate balance of these two families of fats. While a ratio of around 4:1 has for many decades been seen as ‘optimal,' the omega-6 to omega-3 ratio, while useful, has been criticised because it fails to distinguish between long-chain and short-chain omega-6 and omega-3 fatty acids. As the physiological actions of short- and long-chain fatty acids are not equivalent, it is important to acknowledge the individual members of each side of the two families; for example, only the long-chain omega-6, AA and the long-chain omega-3, EPA are precursors to eicosanoids involved in regulating immune, cardiovascular and inflammatory processes. Thus, the AA to EPA ratio is significantly more reflective of the balance of these processes than the omega-6 to omega-3 ratio. As inflammation (more specifically, non-resolving inflammation) is considered to be the driver of common western diseases, the AA to EPA ratio can be used as a biomarker of the body’s inflammatory potential; similarly to the Omega-3 Index, it can be manipulated relatively easily by diet and/or supplements (Rizzo et al. 2010). For example, studies have shown that anti-inflammatory and pro-resolving effects of the downstream products derived from omega-3 (specifically EPA) inhibit atherosclerosis (Bäck & Hansson 2019), with the greatest effects seen once an optimal ‘target’ AA to EPA of 1.3:1 is achieved (Ohnishi & Saito 2013). When considering testing, in addition to the Omega-3 Index (to establish both total and individual EPA & DHA levels) it's important to consider combining this with the AA to EPA ratio to give the complete overview of an individual's health status required to ensure the most appropriate intervention recommendation can be put in place.
The Opti-0-3 fatty acid biomarker test
Growing awareness of the benefits that omega-3 testing can offer has seen a rise of available tests and test kits. The fatty acids within RBCs give a reliable overview of long-term dietary intake; unlike other tests that screen only for a number of ‘significant’ fatty acids and often giving limited information (usually the omega-6 to omega-3 ratio), the Opti-O-3 screens for the full spectrum of fatty acids used to develop and validate the highly published Omega-3 Index (Harris & Von Schacky 2004). From this fatty acid analysis, we provide accurate information on the AA to EPA ratio, the omega-6 to omega-3 ratio and the Omega-3 Index – the three key fatty acid biomarkers related to health. The Omega-3 Index is a useful biomarker for assessing both baseline risk and a change in risk as a result of omega-3 intake. With a strong correlation between the Omega-3 Index and the AA to EPA ratio, by increasing the Omega-3 Index we see a corresponding reduction in AA to EPA. The Opti-O-3 biomarker test is a simple, minimally invasive blood spot test that can be performed by the client at home. As the test doesn't require a phlebotomist to draw blood, it is both cost-effective and convenient and only requires a few drops of blood. Knowledge of the client’s baseline EPA, DHA and AA levels, and their body weight, allows us to offer personalised dosing recommendations using combinations of the omega-3s EPA & DHA and omega-6 GLA designed to reach the target Omega-3 Index of 8-10% and to establish an AA to EPA ratio between 1.5 and 3. This bespoke dosing improves these valuable biomarkers and enables the body to produce the correct balance of the downstream products that are required to ‘switch on, maintain and then switch off’ inflammation appropriately and correctly.
Summary
Most people will significantly overestimate their Omega-3 Index simply because they overestimate their intake of EPA & DHA. This isn’t surprising given that fish isn’t always a reliable source of omega-3 and the majority of fish oils do not provide omega-3 in the dose or form necessary to make a significant impact on raising omega-3 status. Ensuring adequate intake is also challenging when considering that an individual's omega-3 requirements are unique to them; age, level of activity, gender and body weight are all known to influence omega-3 requirements and turnover. The Omega-3 Index is a unique biomarker; unlike cholesterol testing (which is limited to cardiovascular health) it provides valuable information about our overall health, meaning that if we know our omega ‘number’ we take control of our health. The Omega-3 Index has many features that qualify it as not only a biomarker of intake but also as a risk marker and, most importantly, a risk factor and target for intervention. Most people also underestimate (or simply don't know) just how much omega-6 is in their diet. This is significant because when omega-6 dominates, it can dampen the potential benefits of EPA and DHA; importantly, therefore, the Opti-O-3also measures the AA to EPA ratio. Unlike any other test, we also take the guesswork out of supplementing because, unsurprisingly, low baseline values may require a larger dose of EPA and DHA than a high baseline value!
Take the Opti-challenge, find out your number, find out your risk, act to reduce it!
References
Bäck M, Hansson GK. Omega-3 fatty acids, cardiovascular risk, and the resolution of inflammation. FASEB J. 2019 Feb;33(2):1536-1539. doi: 10.1096/fj.201802445R.
Browning LM, Walker CG, Mander AP, West AL, Madden J, Gambell JM, Young S, Wang L, Jebb SA, Calder PC. Incorporation of eicosapentaenoic and docosahexaenoicacids into lipid pools when given as supplements providing doses equivalent to typical intakes of oily fish. Am J Clin Nutr. 2012 Oct;96(4):748-58. Epub 2012 Aug 29.
Fontes JD, Rahman F, Lacey S, Larson MG, Vasan RS, Benjamin EJ, Harris WS, Robins SJ. Red blood cell fatty acids and biomarkers of inflammation: a cross-sectional study in a community-based cohort. Atherosclerosis. 2015 Jun;240(2):431-6.
Flock, M. R., A. C. Skulas-Ray, et al. (2013). "Determinants of erythrocyte omega-3 fatty acid content in response to fish oil supplementation: a dose-response randomized controlled trial." J Am Heart Assoc 2(6): e000513.
Harris WS. Omega-3 fatty acids and cardiovascular disease: a case for omega-3 index as a new risk factor. Pharmacol Res. 2007 Mar;55(3):217-23.
Harris WS, Del Gobbo L, Tintle NL. The Omega-3 Index and relative risk for coronary heart disease mortality: Estimation from 10 cohort studies. Atherosclerosis. 2017 Jul;262:51-54.
Harris WS, Tintle NL, Etherton MR, Vasan RS. Erythrocyte long-chain omega-3 fatty acid levels are inversely associated with mortality and with incident cardiovascular disease: The Framingham Heart Study. J Clin Lipidol. 2018 May - Jun;12(3):718-727.
Jackson KH, Polreis JM, Tintle NL Kris-Etherton PM W.S. Harris WS Association of reported fish intake and supplementation status with the omega-3 index Prostaglandins, Leukotrienes and Essential Fatty Acids Vol. 142 p4–10
Katan MB, Deslypere JP, van Birgelen AP, Penders M, Zegwaard M. Kinetics of the incorporation of dietary fatty acids into serum cholesteryl esters, erythrocyte membranes, and adipose tissue: an 18-month controlled study. J Lipid Res. 1997 Oct;38(10):2012-22.
Laidlaw M, Cockerline CA, Rowe WJ. A randomized clinical trial to determine the efficacy of manufacturers' recommended doses of omega-3 fatty acids from different sources in facilitating cardiovascular disease risk reduction. Lipids Health Dis. 2014 Jun 21;13:99.
Li K, Huang T, Zheng J, Wu K, Li D. Effect of marine-derived n-3polyunsaturated fatty acids on C-reactive protein, interleukin6 and tumor necrosis factor α: a meta-analysis. PLoS One. 2014 Feb 5;9(2):e88103.
Matusheski NV, Marshall K, Hartunian-Sowa S, McBurney MI. US Family Physicians Overestimate Personal ω-3 Fatty Acid Biomarker Status: Associations with Fatty Fish and ω-3 Supplement Intake. Curr Dev Nutr. 2017 Dec 7;2(2):nzx007. https://www.ncbi.nlm.nih.gov/pubmed/30377677
Micha R, Khatibzadeh S, Shi P, Fahimi S, Lim S, Andrews KG, Engell RE, Powles J, Ezzati M, Mozaffarian D; Global Burden of Diseases Nutrition and Chronic Diseases Expert Group NutriCoDE.
Ohnishi H, Saito Y. Eicosapentaenoic acid (EPA) reduces cardiovascular events: relationship with the EPA/arachidonic acid ratio. J Atheroscler Thromb. 2013;20(12):861-77. Epub 2013 Sep 18. Review.
Rizzo AM, Montorfano G, Negroni M, Adorni L, Berselli P, Corsetto P, Wahle K, Berra B. A rapid method for determining arachidonic:eicosapentaenoic acid ratios in whole blood lipids: correlation with erythrocyte membrane ratios and validation in a large Italian population of various ages and pathologies. Lipids Health Dis. 2010 Jan 27;9:7.
Sprague M, Dick JR, Tocher DR. Impact of sustainable feeds on omega-3 long-chain fatty acid levels in farmed Atlantic salmon, 2006-2015. Sci Rep. 2016 Feb 22;6:21892.
Stark KD, Van Elswyk ME, Higgins MR, Weatherford CA, Salem N Jr. Global survey of the omega-3 fatty acids, docosahexaenoic acid and eicosapentaenoic acid in the bloodstream of healthy adults. Prog Lipid Res. 2016 Jul;63:132-52.
Thuppal SV, von Schacky C, Harris WS, Sherif KD, Denby N, Steinbaum SR, Haycock B, Bailey RL. Discrepancy between Knowledge and Perceptions of Dietary Omega-3 Fatty Acid Intake Compared with the Omega-3 Index. Nutrients. 2017 Aug 24;9(9).
von Schacky C. A review of omega-3 ethyl esters for cardiovascular prevention and treatment of increased blood triglyceride levels. Vasc Health Risk Manag. 2006;2(3):251-62. Review.